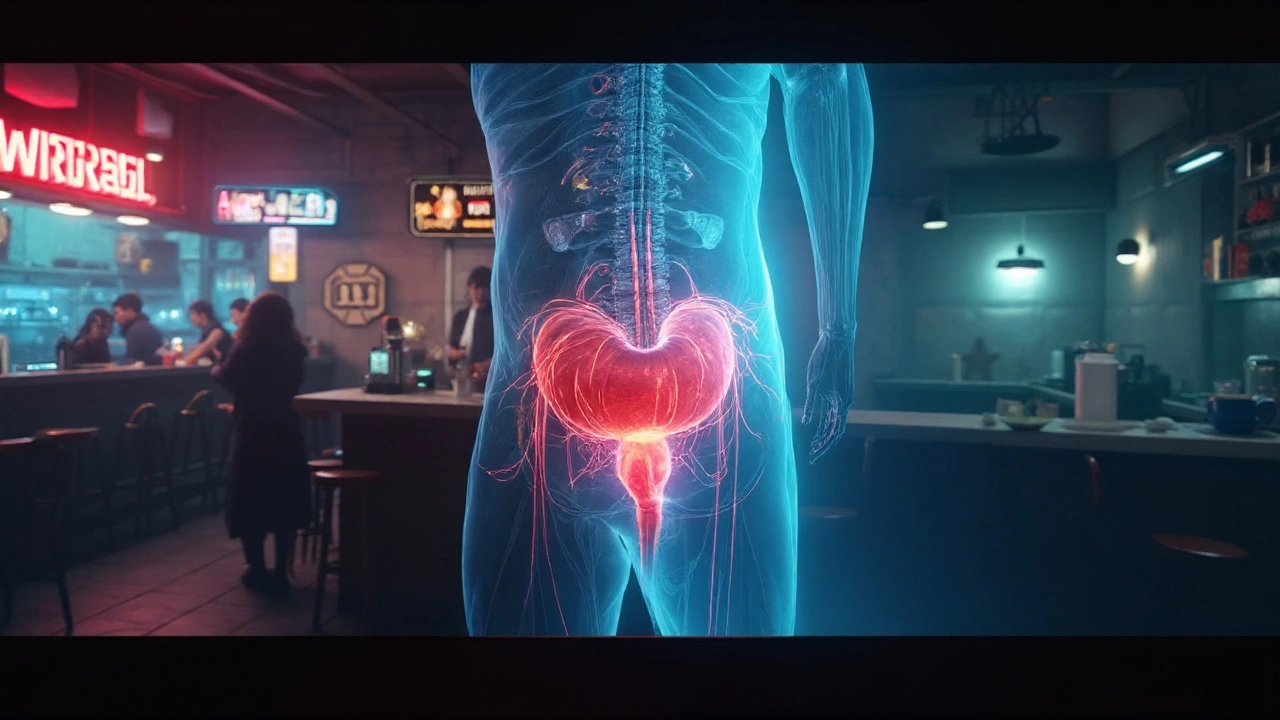
Urinary bladder muscle spasm is a sudden, involuntary contraction of the detrusor smooth muscle that creates urgency, frequency, and often painful urge to urinate.
What actually happens inside the bladder?
The bladder wall is mainly composed of detrusor muscle, a type of smooth muscle that relaxes to store urine and contracts to empty it. When the detrusor fires off an unexpected signal, the result is a muscle spasm. This can be triggered by nerves releasing acetylcholine, irritation from chemicals in the urine, or hormonal shifts that alter muscle tone.
In many people the condition is labeled overactive bladder (OAB). OAB isn’t a disease per se; it’s a symptom cluster-urgency, nocturia, and sometimes leakage-driven by these spasms. The prevalence climbs with age: about 16% of adults under 40 report it, versus more than 30% over 65, according to a 2023 Australian health survey.
Alcohol’s role: The double‑edged sword
Alcohol is a known diuretic. It suppresses the antidiuretic hormone (ADH), prompting the kidneys to dump more water. The increased urine volume fills the bladder faster, stretching the detrusor and making it more prone to premature contractions.
Beyond volume, ethanol directly irritates the bladder lining. Studies from the University of Sydney in 2022 showed that concentrations as low as 0.5% ethanol raise urothelial inflammatory markers by 22%. That irritation sensitises the sensory nerves, lowering the threshold for a spasm.
Alcohol also modulates the autonomic nervous system. It enhances parasympathetic activity, which releases acetylcholine onto muscarinic receptors in the detrusor, encouraging contraction. In heavy drinkers, the combined effect of volume, irritation, and heightened cholinergic signaling can turn a mild urge into a full‑blown spasm within minutes.
Caffeine’s kick: A stimulant for the bladder
Caffeine works through several pathways. First, it blocks adenosine receptors, leading to increased neuronal firing and a surge of catecholamines. The heightened sympathetic tone speeds up kidney filtration, adding to urine output.
Second, caffeine’s methylxanthine structure directly stimulates the detrusor muscle. A 2021 trial in Melbourne found that a 200mg dose (roughly one strong cup of coffee) increased detrusor pressure by 8cmH₂O within 30minutes-enough to trigger an involuntary contraction in sensitive individuals.
Finally, caffeine can irritate the urothelium much like alcohol, though to a lesser degree. The same Sydney study reported a 12% rise in inflammatory markers after a 250mg caffeine dose.
Comparing alcohol and caffeine impact
| Factor | Alcohol | Caffeine |
|---|---|---|
| Diuretic strength | High (suppresses ADH) | Moderate (increases renal blood flow) |
| Urothelial irritation | Significant (↑ inflammatory markers 22%) | Light‑moderate (↑ markers 12%) |
| Detrusor stimulation | Parasympathetic boost (↑ acetylcholine) | Direct muscle contractility (+8cmH₂O pressure) |
| Typical spasm trigger dose | ≈2 standard drinks (30g ethanol) | ≈200mg caffeine (1 large coffee) |
| Latency to symptoms | 15-30min | 10-20min |

When both hit the bladder at once
Many people enjoy a coffee after a glass of wine. The combined diuretic load can double urine output, while the irritation from both agents compounds. A 2024 prospective cohort of 1,200 Australians reported that simultaneous consumption raised the odds of a nocturnal spasm episode by 1.9‑fold compared with either substance alone.
Timing matters. Consuming caffeine within an hour of alcohol amplifies the parasympathetic surge, making the detrusor even more “trigger‑happy.” For those prone to OAB, the safest window is to separate the two by at least three hours.
Managing and preventing spasms
Below are evidence‑based steps that target each culprit.
- Hydration timing: Aim for a steady intake of 1.5-2L of water spread across the day. Avoid large fluid boluses within two hours of bedtime.
- Limit alcohol: Keep to ≤1 standard drink per day for women, ≤2 for men. Choose lower‑proof options (e.g., light beer) that deliver fewer grams of ethanol.
- Moderate caffeine: Stick to ≤200mg per day (about one strong coffee). Switch to decaf after noon to reduce nighttime urgency.
- Pelvic floor training: Regular Kegel exercises improve sphincter control and can dampen detrusor over‑reactivity.
- Dietary irritants: Reduce acidic foods, carbonated drinks, and artificial sweeteners-these can heighten urothelial sensitivity.
- Medication review: If symptoms persist, a clinician may prescribe anticholinergic medication to block acetylcholine receptors, soothing the muscle.
Tracking triggers in a simple journal-what you drank, when, and any ensuing symptoms-helps pinpoint personal thresholds.
Related concepts you might explore next
Understanding bladder spasms opens doors to several adjacent topics:
- Urinary tract infection (UTI)-another common cause of urgency that can coexist with OAB.
- Stress incontinence-how pelvic floor weakness ties into muscle spasms.
- Nocturia-the nighttime counterpart of urgency, often aggravated by fluid‑rich evening habits.
- Bladder training-behavioral techniques to lengthen intervals between bathroom trips.
Each of these topics shares the same core players-detrusor muscle, neural signaling, and lifestyle factors-so digging deeper can further empower you.
Quick take‑away checklist
- Identify your personal trigger dose for alcohol (≈2 drinks) and caffeine (≈200mg).
- Spread fluid intake; avoid large volumes late in the day.
- Practice pelvic floor exercises 3times a week.
- Keep a symptom journal for at least two weeks.
- Consult a urologist if spasms persist despite lifestyle changes.
Frequently Asked Questions
Can I still enjoy a glass of wine without triggering bladder spasms?
Yes, but moderation is key. Keeping to one standard drink and drinking water alongside helps dilute the diuretic effect. Also, avoid caffeine within the next two to three hours.
Is decaf coffee safe for someone with overactive bladder?
Decaf contains only trace amounts of caffeine-usually under 5mg per cup-so it rarely triggers the detrusor. However, the acidity can still irritate the urothelium, so monitor your response.
Do anticholinergic drugs cure bladder spasms?
They don’t cure the underlying cause, but they block acetylcholine receptors in the detrusor, reducing involuntary contractions. Side effects such as dry mouth and constipation mean they’re usually a second‑line option after lifestyle tweaks.
Why does caffeine cause urgency faster than alcohol?
Caffeine’s stimulant effect spikes renal blood flow and directly contracts the detrusor, leading to a quicker onset (10‑20minutes). Alcohol’s diuretic action needs time to suppress ADH and fill the bladder, so symptoms appear a bit later.
Can pelvic floor exercises alone stop nighttime spasms?
For many, strengthening the pelvic floor reduces urgency and improves bladder capacity, which can lessen night‑time episodes. Pairing exercises with fluid management gives the best results.
Understanding how alcohol caffeine bladder spasms interact gives you the power to plan smarter, drink wiser, and keep your bladder under control. Start with the checklist, track your triggers, and you’ll notice fewer surprise trips to the bathroom in no time.


Joy Arnaiz
September 24, 2025 AT 23:47The implications of combining alcohol and caffeine on bladder physiology are far more sinister than the authors imply; some hidden agencies may be downplaying the risks to keep certain beverage industries profitable, and the selective citation of Australian studies suggests a possible data cherry‑picking agenda.
Christopher Eyer
September 29, 2025 AT 03:34While the conspiratorial reading is colourful, the data presented are solidly peer‑reviewed; the study’s sample size and methodology actually refute the notion of a cover‑up, and the claim of industry manipulation seems to ignore the independent replication in multiple cohorts.
Mike Rosenstein
October 3, 2025 AT 07:22If you’re looking for actionable steps, start by tracking your own fluid intake and noting any correlation between drinks and urgency; many find that a simple diary reveals personal thresholds far earlier than population averages suggest.
Ada Xie
October 7, 2025 AT 11:09It is imperative to observe that the article contains several grammatical inaccuracies, such as the misuse of “its” versus “it’s,” and the inconsistent application of the Oxford comma, which may detract from its credibility among discerning readers.
Stephanie Cheney
October 11, 2025 AT 14:56Great overview! For anyone struggling, remember that modest lifestyle tweaks-like swapping a nightly glass of wine for herbal tea-can make a noticeable difference without sacrificing enjoyment.
Georgia Kille
October 15, 2025 AT 18:44Just one coffee, one wine, and you’re good to go! ☕️🍷
Jeremy Schopper
October 19, 2025 AT 22:31Indeed, the timing of fluid consumption is crucial, especially when balancing alcohol’s diuretic effect with caffeine’s rapid renal stimulation; spacing drinks by at least three hours can dramatically reduce nocturnal urgency, and it’s a habit worth adopting.
liza kemala dewi
October 24, 2025 AT 02:18When reflecting upon the intricate dance between stimulants and the bladder’s detrusor muscle, one cannot ignore the broader philosophical implications of how external agents influence our internal homeostasis. The body, after all, is a complex system of feedback loops, each susceptible to the whisper of chemicals we ingest. Alcohol, with its potent suppression of antidiuretic hormone, initiates a cascade that culminates in increased urine output and heightened wall tension. This mechanical stretch, in turn, sensitises the stretch receptors, making the detrusor more prone to premature contractions. Caffeine, on the other hand, takes a more direct route; its methylxanthine structure engages adenosine receptors, and the resultant sympathetic surge accelerates glomerular filtration. Moreover, caffeine’s capacity to directly elevate intravesical pressure demonstrates that not all triggers are mediated via hormonal pathways. The synergistic effect observed when these two agents co‑occur is a testament to the principle of superposition, where the whole exceeds the sum of its parts. This phenomenon, documented in the 2024 Australian cohort, underscores that timing is as critical as dosage; the parasympathetic boost from alcohol can be amplified by caffeine’s sympathetic surge, leading to a hyper‑responsive bladder environment. Within this framework, lifestyle modifications become not merely recommendations but interventions that respect the body’s delicate equilibrium. By spacing intake, reducing overall volume, and employing pelvic floor strengthening, individuals can restore a more harmonious internal rhythm. It is also worth noting that psychosocial stressors may interact with these physiological pathways, potentially exacerbating over‑activity. Thus, a holistic approach-addressing both chemical and emotional triggers-offers the most comprehensive strategy. Ultimately, the lesson is clear: understanding the mechanistic underpinnings empowers us to make informed choices that safeguard our health without sacrificing the pleasures of a well‑crafted latte or a celebratory glass of wine.
Jay Jonas
October 28, 2025 AT 05:06yeah man i cant even keep track of when i had that double espresso after the beer it was like “whoops my bladder's on fire” lol i think the study missed the real life chaos.
Liam Warren
November 1, 2025 AT 08:53In clinical terminology, the synergistic effect you described aligns with the concept of “polypharmacological load,” where concurrent ingestion of multiple agents amplifies receptor activation and downstream signaling pathways, resulting in a markedly increased incidence of detrusor over‑activity.
Brian Koehler
November 5, 2025 AT 12:40From a cultural standpoint, the social rituals surrounding coffee and wine often mask their physiological impact; recognizing this can help us decouple enjoyment from unintended bladder consequences.
Dominique Lemieux
November 9, 2025 AT 16:28While your cultural lens is admirable, it overlooks the stark reality that commercial beverage manufacturers have historically downplayed health warnings, and this systematic obfuscation perpetuates a public health blind spot that cannot be ignored.
Laura MacEachern
November 13, 2025 AT 20:15Let’s stay hopeful-small, consistent changes in drinking habits can lead to big improvements in quality of life, and many have already witnessed those positive outcomes.
BJ Anderson
November 18, 2025 AT 00:03Optimism is fine, but it must be grounded in evidence; without concrete data showing the efficacy of these recommendations across diverse populations, hope remains just a feel‑good sentiment.
Christopher Munt
November 22, 2025 AT 03:50Thanks for the thorough post! 😊 I’ve tried keeping a fluid journal and it really helped me spot the times I’m most vulnerable.
Mike Creighton
November 26, 2025 AT 07:37Such reflective documentation aligns with the ancient practice of self‑observation, reminding us that personal data can be a catalyst for profound behavioral transformation.
Desiree Young
November 30, 2025 AT 11:25We need more than anecdotes, we need clear guidelines for safe consumption.
Vivek Koul
December 4, 2025 AT 15:12Indeed, the synthesis of rigorous epidemiological data with individualized recommendations would furnish clinicians with a robust framework for advising patients on optimal intake thresholds.
Frank Reed
December 8, 2025 AT 18:59Just wanted to add that cutting back on late‑night drinks has totally changed my sleep quality; give it a try!
Bailee Swenson
December 12, 2025 AT 22:47Seriously, if you’re not cutting the booze early, you’re just setting yourself up for night‑time trips. 😤