When you're on a statin to lower cholesterol and then get a bacterial infection, it's easy to assume your doctor will just prescribe any antibiotic. But if that antibiotic is clarithromycin a macrolide antibiotic used to treat respiratory, skin, and other bacterial infections, you could be walking into a dangerous interaction that turns everyday muscle aches into a medical emergency.
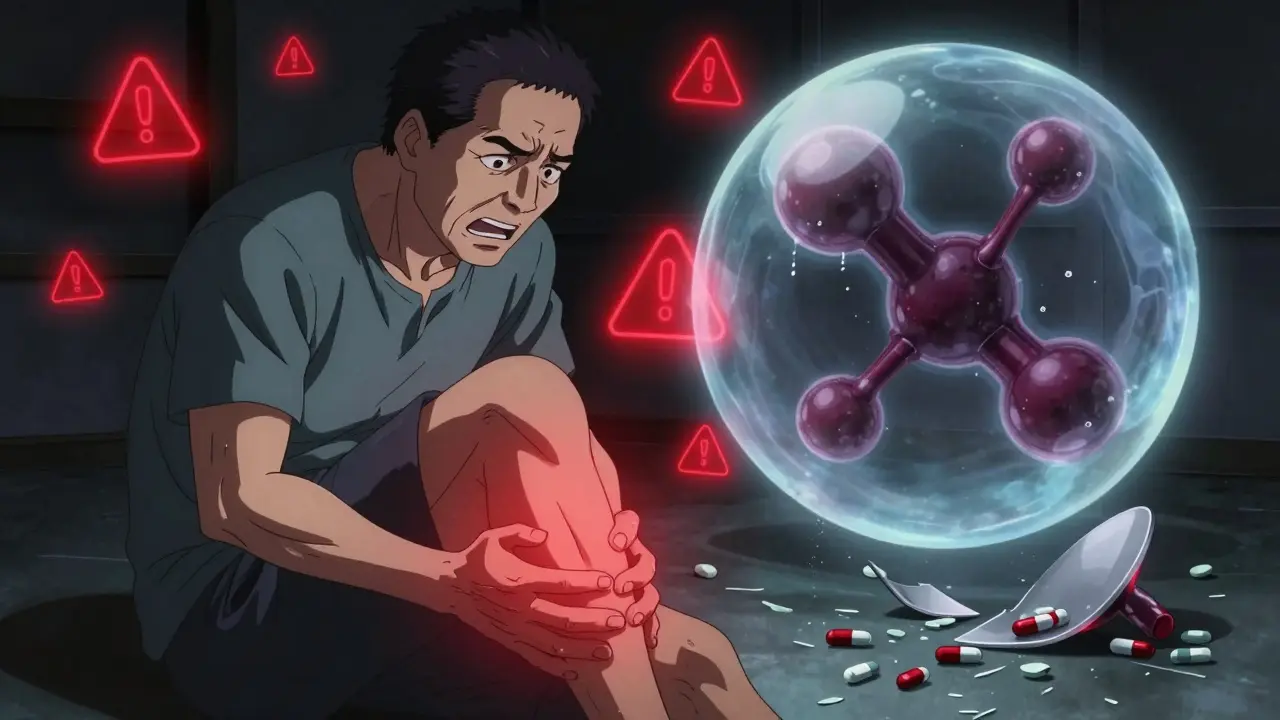
Between 2004 and 2013, the FDA recorded 127 cases of rhabdomyolysis - a life-threatening breakdown of muscle tissue - directly linked to clarithromycin taken with certain statins. That’s not a rare glitch. It’s a predictable, preventable disaster. And it happens because clarithromycin doesn’t just fight bacteria - it also shuts down your body’s ability to break down some of the most common cholesterol drugs.
Why Clarithromycin and Statins Don’t Mix
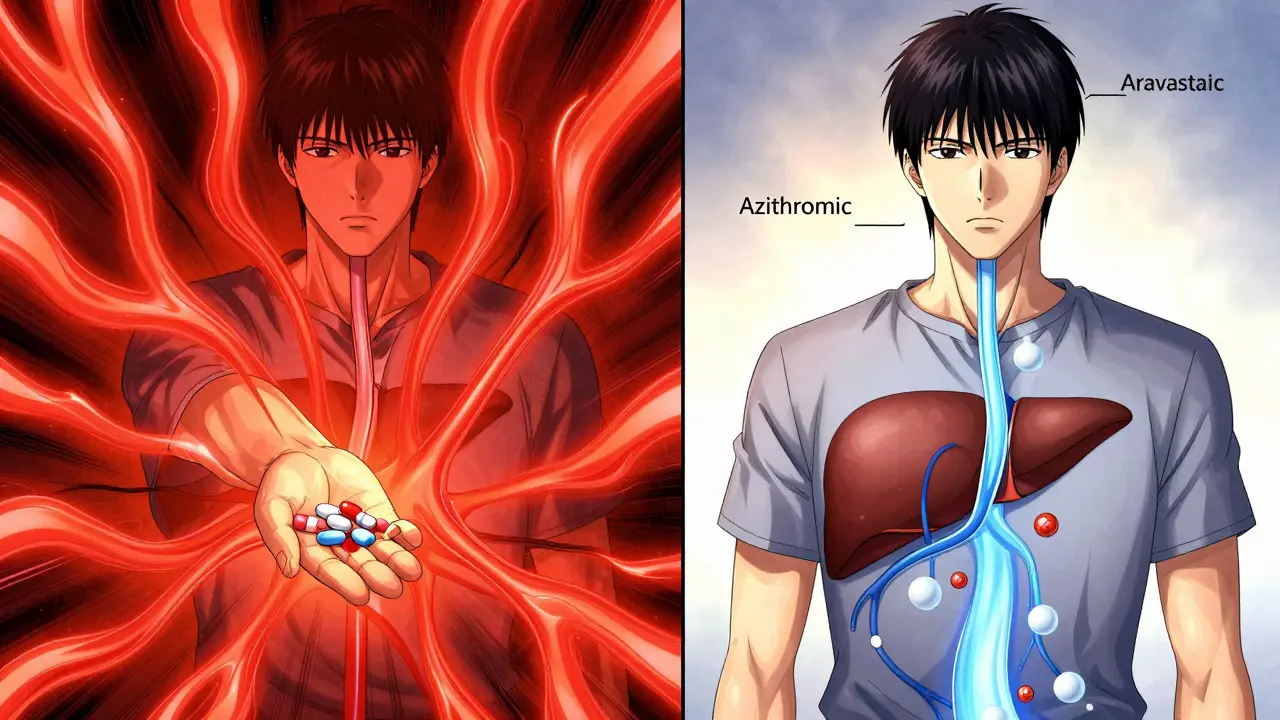
Your liver uses an enzyme called CYP3A4 to process many drugs, including several statins. Clarithromycin doesn’t just pass through your system - it latches onto CYP3A4 like a clog in a pipe. It doesn’t just slow things down. It nearly stops them. That means statins that rely on this enzyme build up in your blood at dangerous levels.
Take simvastatin a statin metabolized almost entirely by CYP3A4, with 95% of its breakdown depending on this enzyme pathway. When you take clarithromycin with it, simvastatin levels in your blood can jump 10 to 12 times higher than normal. That’s not a typo. Tenfold. At that level, muscle cells start dying. Creatine kinase (CK) - a marker of muscle damage - can spike from a normal 60 U/L to over 10,000 U/L. One patient reported CK levels of 12,500 U/L after taking 40 mg of simvastatin with clarithromycin. That’s enough to cause kidney failure.
It’s not just simvastatin. lovastatin another statin heavily dependent on CYP3A4, with plasma concentrations increasing 5- to 20-fold when combined with clarithromycin carries the same risk. Even atorvastatin a statin with moderate CYP3A4 metabolism, showing 4- to 8-fold increases in plasma concentration with clarithromycin isn’t safe at higher doses. The FDA says if you must take both, atorvastatin should never exceed 20 mg daily. But even that carries risk.
Which Statins Are Safer?
Not all statins are created equal when it comes to this interaction. Some barely touch CYP3A4 at all. That’s why your options matter.
- Pravastatin a statin metabolized mainly by sulfation, not CYP3A4, with minimal interaction risk - No dose adjustment needed. One of the safest choices.
- Fluvastatin primarily metabolized by CYP2C9, with little to no CYP3A4 involvement - Low risk. Often overlooked but reliable.
- Rosuvastatin metabolized minimally by CYP2C9, with less than 10% handled by CYP3A4 - Safe up to 20 mg daily, but avoid higher doses.
- Pitavastatin mainly metabolized by glucuronidation, with negligible CYP3A4 involvement - Also low risk, though less commonly prescribed.
These statins are your lifeline if you need an antibiotic. If you’re on simvastatin or lovastatin, your doctor should be asking: Is this really necessary? Because the numbers don’t lie. A 2018 study of over 312,000 patients found the risk of hospitalization for rhabdomyolysis was 4.6 times higher with clarithromycin-simvastatin than with azithromycin-simvastatin.
The Real Danger: It Happens Fast
Most people think drug interactions take weeks to show up. Not this one. Symptoms - muscle pain, weakness, dark urine - can appear as early as day one. On average, they show up by day 3.2. That’s faster than most people realize.
One patient described waking up with pain so severe they needed morphine. Another had CK levels over 200,000 U/L. These aren’t outliers. They’re textbook cases. And they’re avoidable.
Here’s the scary part: a 2022 American Heart Association survey found 68% of statin users had never heard of this interaction. That means most people don’t know they’re at risk. If your doctor prescribes clarithromycin and you’re on a statin, you need to speak up. Don’t wait for symptoms. Ask: Is there a safer antibiotic?
What to Do Instead
The safest fix? Switch the antibiotic.
azithromycin a macrolide antibiotic that does not significantly inhibit CYP3A4, making it the preferred alternative to clarithromycin for statin users is the clear winner. Unlike clarithromycin, azithromycin doesn’t block CYP3A4. A 2013 study in the Canadian Medical Association Journal showed no increased risk of rhabdomyolysis or kidney injury when azithromycin was used with any statin. In fact, patients on azithromycin had lower hospitalization rates than those on clarithromycin.
Here’s what works:
- Ask your doctor to switch from clarithromycin to azithromycin. It’s just as effective for most infections - sinusitis, bronchitis, pneumonia - and far safer with statins.
- If you can’t switch antibiotics, stop your statin during the 5- to 7-day course of clarithromycin. Don’t restart it until 3 to 5 days after you finish the antibiotic. That gives your liver time to clear the inhibitor.
- If you must keep taking the statin, reduce the dose. For simvastatin, cut it to 10 mg. For atorvastatin, don’t go above 20 mg. And get your CK levels checked weekly.
For older adults, people with kidney disease, or those with hypothyroidism, the risk is even higher. In these cases, the American College of Cardiology recommends stopping the statin entirely during clarithromycin treatment.
What to Watch For
You don’t need to be a doctor to spot the warning signs. If you feel any of these, call your doctor immediately:
- Unexplained muscle pain, especially in your shoulders, thighs, or lower back
- Weakness so bad you can’t climb stairs or lift your arms
- Dark, tea-colored urine
- Fever or nausea along with muscle pain
These aren’t "just side effects." They’re signs your muscles are breaking down. Left unchecked, this can lead to kidney failure, dialysis, or even death. The average hospital cost for rhabdomyolysis? $28,500. That’s preventable.
What Your Doctor Should Be Doing
Electronic health records have cut dangerous prescriptions by 42% since 2015. But in 2023, a study in JAMA Internal Medicine found that nearly 19% of primary care doctors still prescribed clarithromycin to patients on high-dose simvastatin. That’s over 132,000 risky prescriptions a year in the U.S. alone.
Your doctor should be checking your medication list before writing any new prescription. If they’re not, ask them. Show them this information. Bring a printed list of your medications. Don’t assume they know.
And if you’re on a statin, keep a wallet card. The American Heart Association offers free ones listing drugs to avoid. Put it in your wallet. Show it to pharmacists. Use it when you’re in the ER.
The Bigger Picture
Statins are among the most prescribed drugs in the world. Over 39 million Americans take them. Clarithromycin is the third most common macrolide antibiotic. That means about 700,000 people in the U.S. are getting this dangerous combo every year. Most don’t know they’re at risk.
But this isn’t just about one drug pair. It’s about how we manage medications. We assume prescriptions are safe together. They’re not. Drug interactions kill. And this one? It’s one of the most predictable.
The future is better. Researchers are now studying genetic factors - like the CYP3A5*3/*3 genotype - that make some people 3.2 times more likely to have muscle damage. Non-systemic antibiotics that don’t touch liver enzymes are in clinical trials. But for now, the fix is simple: avoid the combo. Switch the antibiotic. Or pause the statin. Your muscles will thank you.
Can I take clarithromycin if I’m on a low dose of simvastatin?
Even at 10 mg, simvastatin combined with clarithromycin can raise blood levels by 5- to 8-fold, still putting you at risk for muscle damage. The FDA recommends avoiding this combination entirely. If you must take clarithromycin, stop simvastatin during the course and for 3-5 days after. There are safer alternatives.
Is azithromycin really safer than clarithromycin?
Yes. Azithromycin does not inhibit CYP3A4, so it doesn’t interfere with statin metabolism. Studies show no increased risk of rhabdomyolysis or kidney injury when azithromycin is taken with any statin. It’s the preferred macrolide for patients on statins, according to guidelines from the American Heart Association and Infectious Diseases Society of America.
How long does clarithromycin affect my liver?
Although clarithromycin’s half-life is only 3-7 hours, its active metabolite, 14-OH clarithromycin, lingers for 7-10 days. That means it keeps blocking CYP3A4 for over a week after your last dose. Don’t restart your statin until at least 3-5 days after finishing clarithromycin - and longer if you’re older or have kidney issues.
Should I stop my statin if I need clarithromycin?
Yes, if you’re on simvastatin or lovastatin. For atorvastatin, stopping is strongly advised unless the dose is 20 mg or less and your doctor closely monitors you. For pravastatin, fluvastatin, or rosuvastatin, stopping isn’t usually needed - but still confirm with your doctor. The safest choice is always to pause the statin during and after clarithromycin use.
What if I already took clarithromycin with my statin and now have muscle pain?
Stop the statin immediately. Call your doctor or go to the ER. Get a creatine kinase (CK) blood test. High CK levels (above 1,000 U/L) indicate muscle damage. Dark urine, weakness, or fever mean you may be developing rhabdomyolysis. Don’t wait. This can lead to kidney failure within hours.

Skilken Awe
February 14, 2026 AT 06:00Also, CK levels over 12,500? Congrats, you’ve got a human meat grinder. Now go tell your cardiologist to stop prescribing statins like they’re M&Ms.
Steve DESTIVELLE
February 15, 2026 AT 10:02Stephon Devereux
February 16, 2026 AT 22:25Most people think statins are harmless because they’re common. But this? This is a silent killer that doesn’t care if you’re 65 or 35, rich or insured, smart or not. The fact that 68% of statin users have never heard of this is terrifying.
And azithromycin isn’t just safer-it’s just as effective for 90% of infections. Why are we still defaulting to clarithromycin? Because it’s cheaper? Because it’s habit? Because no one taught us?
Stop waiting for symptoms. Ask the question before the script is written. Carry a meds list. Know your statin. And if your doctor doesn’t know this? Show them this. Print it. Hand it to them. Your muscles are worth it.
athmaja biju
February 18, 2026 AT 20:16Reggie McIntyre
February 19, 2026 AT 20:57Pravastatin? Fluvastatin? Rosuvastatin? I had no idea these even existed. I thought all statins were the same. Turns out, your liver has a VIP list and some drugs just don’t get invited to the CYP3A4 party.
Azithromycin over clarithromycin? That’s like choosing a quiet walk over a mosh pit. Why didn’t anyone tell me this? I’ve been on simvastatin for 7 years. I’m switching today. Thanks for the wake-up call. This isn’t just medical advice-it’s a life hack.
Jack Havard
February 21, 2026 AT 00:48Also, azithromycin has its own risks. QT prolongation. GI issues. Antibiotic resistance. You’re swapping one problem for another. And why is everyone acting like this is new? It’s been in textbooks since the 90s. If you didn’t know, maybe you shouldn’t be on statins at all.
Gloria Ricky
February 21, 2026 AT 03:56This post saved us. I’m calling his doctor tomorrow to switch him to pravastatin. Thank you for writing this. Not everyone gets how scary this is. You made it real. I’m printing this out and putting it on the fridge. No one should go through what he did.
Stacie Willhite
February 22, 2026 AT 17:39Thank you for being so clear. I’m going to print the list of safe statins and keep it in my wallet. I’m also going to ask my pharmacist next time I refill. I never thought to ask. I just trusted.
This feels like a quiet victory. Knowledge is armor. And now I’m armored.
Jason Pascoe
February 24, 2026 AT 06:10What’s wild is how often the patient doesn’t even know they’re on a statin. Elderly folks get statins prescribed by a cardiologist, then get antibiotics from urgent care 3 weeks later-no one talks.
Simple fix: always ask: "Is this statin on the CYP3A4 list?" And if the answer is yes, don’t reach for clarithromycin. Azithromycin works just as well. No drama. No hospitalization. Just good care.
Sonja Stoces
February 25, 2026 AT 12:36And why is azithromycin suddenly the golden child? It’s been linked to sudden cardiac death in high-risk patients. You’re trading one risk for another.
Also, 19% of doctors still prescribe this combo? Wow. That’s 19% more than the 0% who should.
Meanwhile, the real problem is that we treat drugs like they’re interchangeable Lego blocks. We need better systems. Not more pamphlets.
Gabriella Adams
February 26, 2026 AT 01:43Here’s the truth: if you’re over 65, diabetic, or have renal impairment, and you’re on simvastatin or lovastatin? You’re playing Russian roulette with your kidneys.
But here’s the good news: you can fix this. TODAY.
Ask for azithromycin. Ask for pravastatin. Ask for a CK test. Ask. Ask. Ask.
And if your doctor says, ‘It’s fine’? Get a second opinion. Your muscles are not disposable. Your kidneys aren’t replaceable. And your life? It’s worth the conversation.