Imagine lying awake at 3 a.m., heart pounding, air mask tight on your face, wondering why you’re still tired even though you’re using your CPAP machine every night. You’ve been told you have sleep apnea - but the insomnia won’t leave. This isn’t just bad luck. It’s COMISA - Comorbid Insomnia and Sleep Apnea - and it’s far more common than most doctors realize.
What Exactly Is COMISA?
COMISA isn’t just having two sleep problems at once. It’s when insomnia and obstructive sleep apnea (OSA) feed off each other, making both worse. You might fall asleep easily but wake up 10 times a night because your airway collapses. Or you might lie there for hours, too anxious to sleep, while your body struggles to breathe. The result? Exhaustion that doesn’t go away, no matter how long you stay in bed. Research from Flinders University in Australia shows that between 39% and 58% of people diagnosed with sleep apnea also have clinical insomnia. That’s nearly half of all OSA patients. Yet, most clinics still treat them as separate issues - first fix the breathing, then deal with the sleeplessness. That approach often fails.Why Standard Treatments Fall Short
CPAP therapy is the gold standard for sleep apnea. When used correctly, it works 85-90% of the time. But in COMISA patients, adherence drops to just 42.7%. Why? Because the mask itself can trigger or worsen insomnia. The pressure, the noise, the feeling of being trapped - all of it makes it harder to fall asleep. One patient on Reddit put it simply: “The machine that’s supposed to help me sleep is the reason I can’t.” On the flip side, cognitive behavioral therapy for insomnia (CBT-I) is highly effective for pure insomnia, helping 70-80% of people. But if you’re still having breathing pauses every night, no amount of sleep hygiene or stimulus control will fix the root problem. You’ll still wake up gasping, your brain still in survival mode. Treating one condition without the other is like trying to fix a car with a broken engine by just changing the tires. It might look better, but it won’t go anywhere.The Proven Solution: CBT-I + CPAP Together
The breakthrough came when researchers stopped treating these as separate problems and started treating them as one. Dr. Alexander Sweetman’s work at Flinders University showed that combining CBT-I with CPAP from day one leads to dramatically better outcomes. In a major clinical trial, patients who got both treatments saw a 63% reduction in insomnia symptoms after 12 weeks. Those who only got CPAP? Only 29% improved. Even more striking: CPAP usage increased by an average of 1.2 hours per night when CBT-I was added. That’s not a small gain - it’s the difference between barely surviving the night and actually sleeping. CBT-I doesn’t just help you sleep better. It helps you tolerate CPAP better. Techniques like sleep restriction (limiting time in bed to match actual sleep time) train your brain to associate the bed with sleep, not frustration. Stimulus control teaches you to get out of bed if you’re not sleeping - which reduces the anxiety of lying there with a mask on. And relaxation training lowers the stress response that keeps your body tense, even when your airway is open.Who Needs This Approach?
Not everyone with sleep apnea has COMISA. But if you’ve been on CPAP for more than a few weeks and still feel exhausted, have trouble falling asleep, or wake up frequently without knowing why, you might have it. Diagnostic criteria are clear: you need a sleep study (polysomnography) showing an Apnea-Hypopnea Index (AHI) of 5 or higher, plus an Insomnia Severity Index (ISI) score of 15 or above. That’s not just “I had a rough night.” That’s insomnia severe enough to impact your mood, focus, and daily life. The type of insomnia matters too. About 68% of COMISA patients struggle with sleep maintenance - waking up and not being able to fall back asleep. That’s different from sleep onset insomnia (trouble falling asleep at the start of the night), which makes up the other 32%. CBT-I protocols can be adjusted for each type, making treatment more precise.
What If You Can’t Get CBT-I?
Access is still a major barrier. Only 12% of patients report having access to a psychologist trained in CBT-I for COMISA. Wait times can stretch to 14 weeks. But there are options. Digital CBT-I platforms like Sleepio and Somryst now offer COMISA-specific modules. These are not generic apps - they’re designed to integrate CPAP usage data and adjust therapy based on your nightly breathing patterns. A 2023 study in JAMA Network Open found these platforms helped 65% of mild COMISA cases (AHI 5-15) achieve insomnia remission. For moderate to severe cases (AHI >15), the success rate drops to 38%, so they’re not a full replacement - but they’re a bridge. Some patients benefit from gradual CPAP adaptation. Instead of starting at full pressure, devices like ResMed’s AirSense 11 allow for ramping - slowly increasing pressure over 20-45 minutes. Combine that with a consistent bedtime routine and avoiding screens before bed, and many see big improvements.What About Medications or Other Devices?
Medications like suvorexant, an orexin antagonist approved by the FDA in December 2023 for COMISA, show promise. In trials, it improved sleep maintenance by 42% when paired with CPAP. But it’s not a first-line treatment. It’s expensive, can cause next-day drowsiness, and doesn’t fix the underlying behavioral patterns that keep insomnia going. Mandibular advancement devices work for mild to moderate OSA, but they don’t help with insomnia. Neurostimulation devices are still experimental. The bottom line: nothing else comes close to the evidence behind combined CBT-I and CPAP.Why Most Doctors Still Miss This
Primary care doctors, sleep labs, and even some sleep specialists still treat these conditions in silos. A patient with loud snoring gets a CPAP referral. A patient with trouble sleeping gets a referral to a therapist. Few are trained to look for both. A 2022 survey of U.S. sleep centers found that 63% had no formal system to refer OSA patients to behavioral sleep specialists. Only 28% had any kind of coordinated care pathway. That’s why the average COMISA patient waits 7.2 years to get the right diagnosis. The American Academy of Sleep Medicine updated its guidelines in 2023 to explicitly recommend combined treatment. But guidelines don’t change practice overnight. It takes training, funding, and coordination - things most clinics still lack.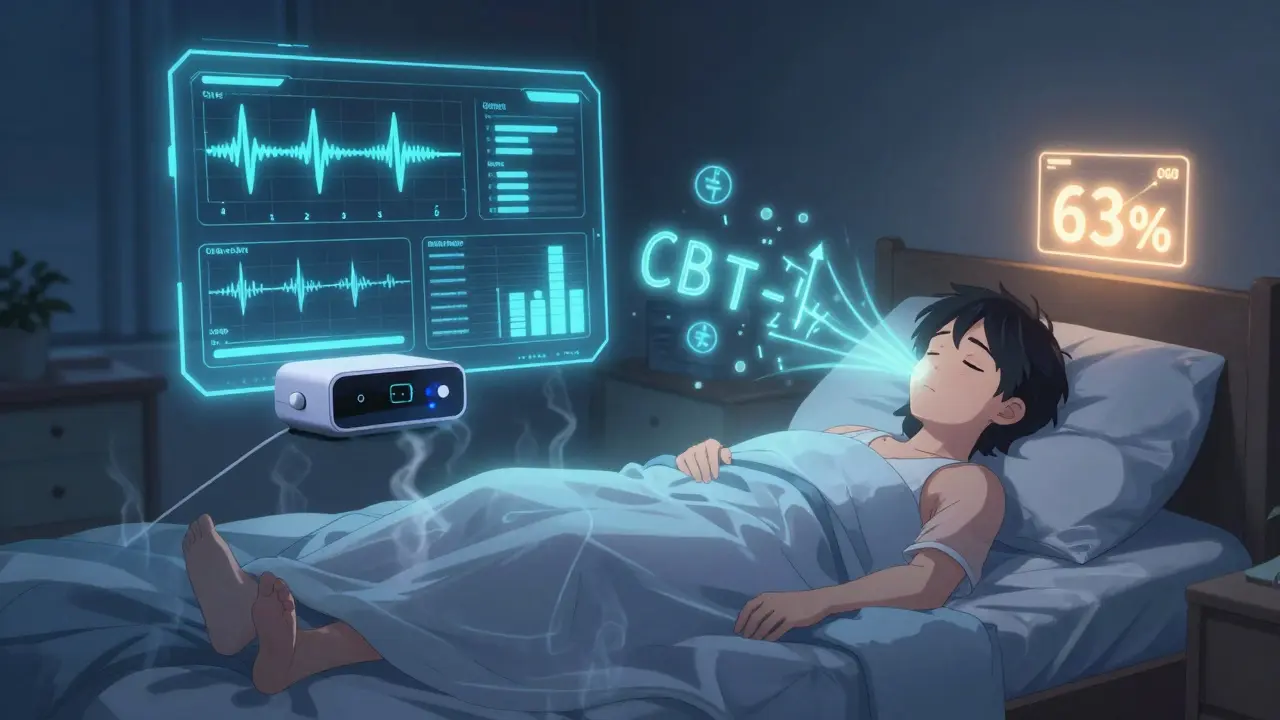
What’s Changing - and What’s Next
Things are moving. In January 2024, Medicare added new billing codes (G2212-G2214) specifically for integrated COMISA treatment. That means clinics can now get paid for bringing together sleep physicians and psychologists. UnitedHealthcare reported $1,843 in annual savings per patient when COMISA was treated properly - because fewer ER visits, fewer missed workdays, fewer depression diagnoses. Researchers are now using AI to predict who’s at risk for COMISA before it becomes severe. A 2023 model developed by Sweetman’s team can predict COMISA with 78% accuracy using just sleep logs, symptom reports, and basic health data. Home-based diagnostic tools that test for both breathing disruptions and sleep fragmentation are in development. Soon, you might be able to get a full COMISA diagnosis from a single overnight test at home.What You Can Do Right Now
If you suspect you have COMISA:- Track your sleep for two weeks - note when you fall asleep, wake up, and how rested you feel.
- Use your CPAP consistently for at least 4 hours a night. Don’t quit because of discomfort - it gets better.
- Ask your sleep doctor for an Insomnia Severity Index (ISI) test. If your score is 15 or higher, ask about CBT-I.
- If you can’t see a specialist, try a digital CBT-I program that’s designed for COMISA (look for one that integrates with your CPAP data).
- Don’t accept “just live with it.” Your fatigue isn’t normal. Your sleep isn’t broken beyond repair.
Final Thought: You’re Not Alone
You’re not failing because you can’t sleep with a mask on. You’re not weak because you’re still tired after months of treatment. You have a complex, under-recognized condition that requires a smarter approach - not more willpower. The science is clear: treating insomnia and sleep apnea together works. The systems are slowly catching up. And you? You’re already ahead of the curve just by asking the right questions.Is COMISA the same as having insomnia and sleep apnea separately?
No. COMISA is a specific clinical syndrome where insomnia and obstructive sleep apnea interact in a way that makes both worse. Treating them separately often fails because the symptoms feed into each other - for example, CPAP discomfort can worsen insomnia, and chronic sleeplessness can increase airway collapse during sleep. COMISA requires a combined treatment approach.
Can I treat COMISA with just a CPAP machine?
CPAP alone treats the breathing issues but doesn’t fix insomnia. In fact, up to 39% of OSA patients on CPAP still report persistent insomnia. Without addressing the sleep maintenance or sleep onset problems, CPAP adherence drops significantly. Combined treatment with CBT-I improves both sleep quality and CPAP usage.
What is CBT-I, and how does it help with sleep apnea?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a structured program that changes thoughts and behaviors around sleep. It doesn’t directly fix breathing pauses, but it reduces the anxiety and hyperarousal that make you wake up from them. It also improves your tolerance for CPAP by teaching you to associate your bed with rest, not frustration. Studies show CBT-I can reduce OSA severity by up to 15% by consolidating sleep and reducing nighttime awakenings.
How do I know if I have COMISA?
You need two things: a sleep study showing an AHI of 5 or higher (indicating sleep apnea), and a score of 15 or higher on the Insomnia Severity Index (ISI). If you’ve been on CPAP for weeks and still can’t fall or stay asleep, or if you were diagnosed with insomnia but snore loudly or wake up gasping, you may have COMISA. Ask your doctor for both tests.
Are digital CBT-I apps effective for COMISA?
Yes - but with limits. Digital CBT-I platforms like Sleepio and Somryst work well for mild COMISA (AHI 5-15), helping 65% of users achieve insomnia remission. For moderate to severe OSA (AHI >15), success drops to 38%. These apps are best used as a bridge to in-person care or when specialists aren’t available. Look for platforms that sync with your CPAP device for better results.
Why is it taking so long for doctors to treat COMISA properly?
Most sleep clinics are set up to treat one condition at a time. There’s little coordination between sleep labs and behavioral health providers. Only 28% of U.S. sleep centers have formal referral pathways for COMISA. Training, funding, and insurance reimbursement have lagged behind the science - but that’s changing. New Medicare codes introduced in 2024 now pay for integrated care, which should speed up adoption.
What’s the biggest mistake people make with COMISA?
Giving up on CPAP because of insomnia - or waiting to treat insomnia until after CPAP “works.” Neither approach works. The longer you delay combining treatments, the more your brain learns to associate the bed with frustration. The sooner you start both CBT-I and CPAP together, the faster you’ll get real, lasting sleep.


Donna Packard
December 18, 2025 AT 03:24Chris Van Horn
December 19, 2025 AT 11:57Raven C
December 21, 2025 AT 10:42Naomi Lopez
December 22, 2025 AT 08:31Sachin Bhorde
December 23, 2025 AT 18:30Salome Perez
December 24, 2025 AT 19:58Marie Mee
December 25, 2025 AT 02:26Kaylee Esdale
December 25, 2025 AT 16:27Joe Bartlett
December 25, 2025 AT 18:08Jody Patrick
December 27, 2025 AT 16:44Radhika M
December 28, 2025 AT 18:08Meghan O'Shaughnessy
December 29, 2025 AT 22:05Michael Whitaker
December 30, 2025 AT 09:02Patrick A. Ck. Trip
January 1, 2026 AT 04:04Virginia Seitz
January 2, 2026 AT 05:18