When you start a new medication for depression, anxiety, or another mental health condition, you’re hoping for relief-not a new set of problems. But for many people, one of the most common and least talked-about side effects is sexual dysfunction. It’s not rare. In fact, between 58% and 70% of people taking antidepressants experience some form of sexual side effect. That’s more than half. And yet, most patients say their doctor never mentioned it before prescribing the drug.
What Sexual Side Effects Actually Look Like
Sexual side effects don’t look the same for everyone. For men, the most common issues are losing interest in sex, trouble getting or keeping an erection, and delayed or absent orgasm. For women, it’s often low desire, pain during sex, or being unable to reach orgasm. These aren’t just inconvenient-they can damage relationships, lower self-esteem, and make people feel broken when they’re not. Some medications are far more likely to cause these problems than others. SSRIs like fluoxetine, sertraline, and paroxetine are the biggest offenders, affecting up to 70% of users. But not all antidepressants are the same. Bupropion (Wellbutrin) and mirtazapine (Remeron) have much lower rates-around 5% to 10%. That’s a huge difference. And if you’re on an antipsychotic that raises prolactin levels, you might experience sexual side effects too. Switching to aripiprazole can help in up to 75% of those cases. Here’s the tricky part: up to half of people with untreated depression already have sexual problems before they even start medication. So when you notice changes after starting a new drug, it’s not always clear whether it’s the illness or the treatment causing it. That’s why tracking your baseline before starting medication matters.Why Most People Don’t Talk About It
Embarrassment is the biggest barrier. A survey by NAMI found that 73% of patients who experienced sexual side effects waited an average of over four months before telling their doctor. Why? They assumed nothing could be done. Or worse-they thought it was their fault. Doctors don’t bring it up much either. On Reddit’s mental health forum, 68% of respondents said their prescriber never mentioned sexual side effects before prescribing. In a JAMA survey, 64% of medical residents admitted they felt uncomfortable discussing sex with patients. But silence doesn’t protect anyone. It just lets problems grow. When providers do talk about it, the results are different. Patients whose doctors explained the risks upfront and offered solutions reported 82% satisfaction with treatment. Those who didn’t? Only 47%. It’s not about scaring people. It’s about preparing them.What Works: Proven Strategies to Fix It
There are six evidence-backed ways to handle this, and you don’t have to just live with it.- Dose reduction: Lowering the dose helps 25-30% of people without losing the antidepressant effect.
- Drug holidays: Skipping the pill for 2-3 days before sex can work for 40% of users-but only if your medication has a short half-life. Paroxetine? Not ideal. Sertraline? More manageable.
- Switching medications: Going from an SSRI to bupropion or mirtazapine works in 65-70% of cases. One patient shared: “My sex life improved within two weeks after switching. I’ve stayed on treatment for 18 months now.”
- PDE5 inhibitors: Sildenafil (Viagra) helps with erections in 55-60% of men, but it doesn’t fix low desire or delayed orgasm. And if you’re not told how to use it properly, it won’t work.
- Sexual scheduling: Planning sex for times when the medication’s effects are weakest-like early morning before the daily dose-helps 35% of couples.
- Couples therapy: When sexual side effects strain a relationship, therapy improves outcomes in half the cases.
How Counseling Should Work
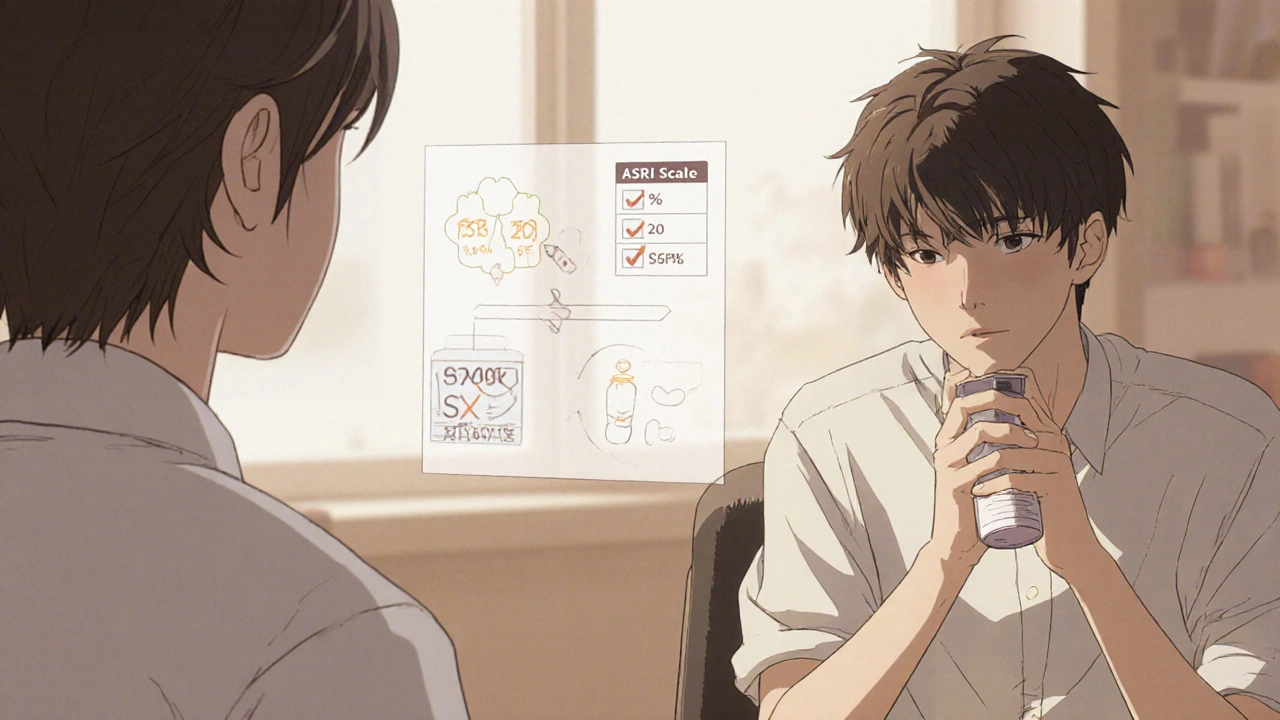
Good counseling isn’t a one-time warning. It’s a process. Start with a quick baseline check. The Arizona Sexual Experience Scale (ASEX) takes less than seven minutes. Ask: “Have you noticed any changes in your desire, arousal, or orgasm?” Record it. Then, before prescribing, say: “About 6 out of 10 people on this medication notice changes in their sex life. It doesn’t happen to everyone, but it’s common enough that we plan for it.” Follow up at 2, 4, and 6 weeks. Don’t wait for the patient to bring it up. Ask directly: “How’s your sex life been since we started this?” If they say nothing’s changed, dig deeper. “Have you felt less interested in sex? Any trouble with arousal or orgasm?” Have a plan ready. If side effects show up, don’t say, “It’ll pass.” Say: “Here are your options. We can lower the dose, switch to a different drug, add a medication to help, or try timing sex differently.” Pharmacists can help too. They’re often the ones handing out the pill bottle. With proper training, they can spot problems early and offer simple solutions. Programs like the American Society of Health-System Pharmacists’ sexual health module have boosted pharmacist confidence by 35%.What’s Changing-and What’s Not
The tide is turning, slowly. The American Psychiatric Association now requires routine sexual function checks in depression treatment guidelines. The FDA requires clearer warnings on antidepressant labels. Telehealth platforms like Ro and Hims now offer specialized services for this exact issue. In 2023, 62% of major health systems started screening for sexual side effects as part of standard care. But gaps remain. Only 38% of U.S. insurance plans cover sex therapy. LGBTQ+ patients are 28% less likely to have these conversations with providers. And research still focuses mostly on men. Only 12% of clinical trials on sexual dysfunction include women as the primary focus. New treatments are on the horizon. A drug targeting the 5-HT2C receptor is in phase 3 trials and could counteract SSRI-induced sexual dysfunction without reducing antidepressant effects. Results are expected in early 2024.What You Can Do Right Now
If you’re on medication and noticing changes in your sex life:- Don’t stop taking your pill without talking to your doctor.
- Write down exactly what’s changed-desire, arousal, orgasm, pain, timing.
- Bring it up at your next appointment. Say: “I’ve noticed changes in my sex life since starting this medication. What can we do?”
- Ask if switching to bupropion or mirtazapine is an option.
- If you’re a man with erection issues, ask if sildenafil might help-and how to use it correctly.
- Consider couples counseling if your relationship is strained.
- Use ASEX or a simple two-question screen before prescribing.
- Normalize the conversation: “This happens to a lot of people. We can fix it.”
- Set automatic follow-ups at 2, 4, and 6 weeks to check sexual function.
- Keep a list of alternatives ready: dose changes, switches, adjuncts.
- Partner with your pharmacy team. They’re your ally.
It’s Not Just About Sex
Sexual side effects aren’t a footnote in treatment. They’re a major reason people quit their medication. And when they stop, their depression often comes back harder. This isn’t about being sexual. It’s about being whole. It’s about feeling like yourself again-not just emotionally, but physically. It’s about connection, intimacy, and dignity. The science is clear. The solutions exist. The only thing missing is the conversation. Start it.Do all antidepressants cause sexual side effects?
No. SSRIs like fluoxetine and sertraline cause sexual side effects in 50-70% of users. But bupropion (Wellbutrin) and mirtazapine (Remeron) affect only 5-10% of people. Some antipsychotics can cause them too, especially if they raise prolactin levels. Not all medications are the same.
Can I just stop taking my medication if sex life suffers?
Don’t stop abruptly. Stopping suddenly can cause withdrawal symptoms and make your depression worse. Talk to your doctor first. There are safer options: lowering your dose, switching medications, adding a supplement, or adjusting timing. You don’t have to choose between mental health and sexual health.
Is it my fault if I lose interest in sex after starting medication?
Absolutely not. This is a known, common side effect of many psychiatric medications-not a personal failure. Studies show up to 70% of people on SSRIs experience this. It’s biology, not character. Many patients feel guilty, but the problem lies with the medication’s effect on neurotransmitters, not your desire or worth.
How long do sexual side effects last?
For some, they go away after a few weeks as the body adjusts. For others, they persist as long as the medication is taken. That’s why proactive management matters. If side effects last beyond 6 weeks and bother you, don’t wait. Ask about alternatives. Delaying action increases the risk of quitting treatment entirely.
Can my partner help me deal with this?
Yes. Open communication with your partner reduces shame and builds support. Couples therapy focused on sexual health improves outcomes in about half of cases where relationship strain has developed. You don’t have to face this alone. Involving your partner can turn a source of stress into a shared solution.
Why don’t doctors talk about this more?
Many providers feel uncomfortable discussing sex, especially in short appointments. Others assume patients won’t bring it up, so they don’t either. But research shows that when doctors initiate the conversation, patients are more likely to report side effects and stay on treatment. It’s not about lack of knowledge-it’s about lack of routine practice.
Are there any new treatments coming for this?
Yes. A new drug targeting the 5-HT2C receptor is in late-stage trials and aims to reverse SSRI-induced sexual dysfunction without reducing antidepressant effects. Results are expected in early 2024. Also, digital tools like the MoodFX app now track sexual function alongside mood, helping patients and providers spot problems early.
Is this issue worse for women than men?
Women experience sexual side effects just as often, but research has focused mostly on male symptoms like erectile dysfunction. Women’s issues-low desire, pain during sex, anorgasmia-are less studied and less understood. Only 12% of clinical trials on sexual dysfunction specifically focus on women. That gap means fewer targeted solutions exist for them right now.

Kristina Williams
November 17, 2025 AT 17:21Yeah right, like the government isn’t secretly using SSRIs to make people docile and uninterested in sex so they don’t rebel. I read a guy on 4chan who said the FDA’s been hiding this since the 90s. They don’t want you horny, they want you compliant. And don’t even get me started on the pharma ads-always smiling people holding coffee, never showing the guy crying in the bathroom because he can’t get it up after his ‘miracle pill.’
Shilpi Tiwari
November 18, 2025 AT 15:00From a pharmacodynamic standpoint, the 5-HT2C receptor antagonism pathway is the critical mediator here-SSRIs induce prolonged serotonergic tone, which downregulates dopaminergic signaling in the mesolimbic circuitry, thereby suppressing libido and orgasmic threshold. The fact that bupropion’s NDRI profile avoids this is mechanistically elegant. But what’s the clinical translatability of ASEX scores in low-resource settings? Most of us don’t have access to validated scales, just a Google form and a prayer.
Christine Eslinger
November 20, 2025 AT 00:08This is one of those topics that gets buried because it’s ‘awkward,’ but it’s literally about quality of life. If you’re taking a pill to feel like yourself again, and it makes you feel less like a person-less connected, less alive-that’s not progress. I’ve been on mirtazapine for two years now, and my sex life? Better than ever. I wish my doctor had told me about alternatives before I suffered through six months of SSRIs. You’re not broken. The drug might be the problem. And there are better options. Please, don’t suffer in silence. Ask. Push. Advocate. You deserve to feel whole.
Holly Powell
November 21, 2025 AT 17:52Let’s be real-most people who complain about sexual side effects are just bad at managing expectations. If you can’t handle a little neurochemical recalibration, maybe you shouldn’t be on psychotropics in the first place. And couples therapy? That’s just a fancy way of saying ‘my relationship is crumbling because I’m too lazy to take responsibility.’ Also, the FDA’s warnings are fine, but the real issue is patients who think medication is a magic wand, not a tool. Stop blaming the drug. Start owning your biology.
Emanuel Jalba
November 22, 2025 AT 02:54OMG I CRIED WHEN I READ THIS 😭 I WAS ON ZOLOFT FOR 3 YEARS AND MY BF LEFT ME BECAUSE I ‘WASN’T INTO IT’ 😭😭😭 BUT THEN I SWITCHED TO WELLBUTRIN AND NOW WE’RE MORE INTIMATE THAN EVER 😍❤️🔥 I’M NOT JUST A PATIENT-I’M A PERSON AGAIN!!
Hal Nicholas
November 23, 2025 AT 12:31Everyone’s acting like this is some new revelation. I’ve been on SSRIs since 2010. The sexual side effects? Always there. The fact that doctors still don’t mention it? Pathetic. And don’t get me started on ‘drug holidays’-that’s a joke unless you’re on sertraline. Paroxetine? No. You’ll get brain zaps and nightmares. This article reads like a pharma pamphlet dressed up as journalism. Real talk: if you’re not willing to switch meds or go off them entirely, you’re just delaying the inevitable collapse. And yes, I’ve tried everything. None of it’s perfect.
Louie Amour
November 25, 2025 AT 11:05You people are so naive. You think this is about sex? Nah. It’s about control. The pharmaceutical industry doesn’t want you feeling powerful, confident, or sexually liberated. They want you docile, medicated, and dependent. That’s why they push SSRIs over bupropion-it’s more profitable to keep you on a drug that makes you numb in every way. And now they’re selling you ‘couples therapy’ like it’s a fix? Please. They’re selling you the illusion of choice. The real solution? Stop trusting the system. Go off the meds. Find a naturopath. Or better yet-get off the grid. Your libido isn’t broken. The system is.
Denny Sucipto
November 25, 2025 AT 11:59Hey-I’ve been there. Took fluoxetine for a year, felt like a ghost in my own body. Didn’t tell anyone. Thought I was broken. Then I found a therapist who asked me about sex on the third visit. I cried. She didn’t flinch. We switched me to bupropion. Two weeks later, I kissed my partner for the first time in months and actually felt it. Not just the touch-the connection. You’re not alone. It’s not your fault. And it’s not permanent. Talk to someone. Even if it’s just one person. You deserve to feel alive in every way. I’m rooting for you.