Macrolide ECG Risk Calculator
Risk Assessment Tool
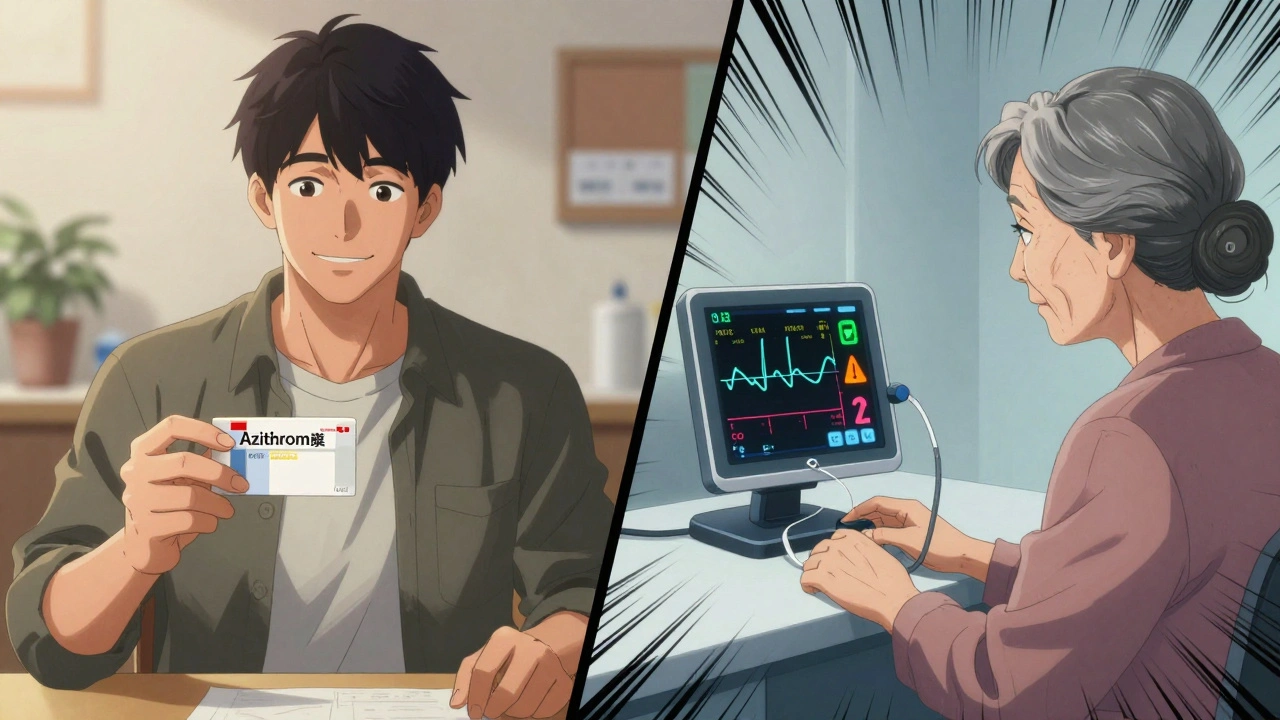
Calculate your risk of QT prolongation when taking macrolide antibiotics like azithromycin or clarithromycin based on key medical factors.
Risk Assessment Result
Why ECG Monitoring Matters When You’re on Macrolides
Macrolide antibiotics like azithromycin, clarithromycin, and erythromycin are among the most commonly prescribed antibiotics for pneumonia, bronchitis, and sinus infections. But behind their effectiveness lies a quiet danger: they can stretch out the heart’s electrical cycle, measured as the QT interval on an ECG. When that interval gets too long, it can trigger a deadly heart rhythm called Torsades de Pointes. It’s rare-but when it happens, it’s often sudden, and sometimes fatal.
So who needs an ECG before starting these drugs? Not everyone. But too many people are getting them anyway-without any screening-and that’s where the real risk hides.
The Real Risk: QT Prolongation Isn’t Just a Lab Finding
Macrolides block a specific potassium channel in the heart (hERG), slowing down the electrical reset between beats. That’s what causes the QT interval to lengthen. Erythromycin has the strongest effect-nearly five times the risk compared to safer alternatives. Azithromycin, the most popular one, carries a smaller but still real risk: a 2.7 times higher chance of cardiovascular death than amoxicillin, according to a major 2012 study in the New England Journal of Medicine.
The danger spikes when the corrected QT interval (QTc) hits 500 milliseconds or more. For every extra 10 ms beyond that, the chance of a life-threatening arrhythmia goes up by 5-7%. That’s not theoretical. A 2025 study in Biomedicines confirmed this curve holds true across thousands of patients.
But here’s the catch: the absolute risk is low-only 1 to 8 cases per 10,000 patient-years. That’s why many doctors think, “It’s rare, so why bother?” But rarity doesn’t mean irrelevance. One preventable death is one too many.
Who’s at Highest Risk? The 14 Warning Signs
ECG monitoring isn’t about blanket screening. It’s about targeting the people who actually need it. The American Heart Association and NIH now agree: risk stratification is key. Here’s who’s most vulnerable:
- Women (risk is nearly 3 times higher than in men)
- People over 65 (risk more than doubled)
- Those with kidney or liver disease (drugs build up in the body)
- Patients already on other QT-prolonging drugs-like certain antidepressants, antifungals, or antiarrhythmics (risk jumps 4 times)
- People with a history of heart disease, heart failure, or prior arrhythmias
- Those with low potassium or magnesium levels
- Patients taking high doses or long courses of macrolides
- Anyone with a family history of sudden cardiac death or inherited Long QT Syndrome
It’s not about being “healthy.” It’s about stacking risk factors. A 70-year-old woman with mild kidney impairment on azithromycin and a diuretic? That’s a red flag. A 30-year-old man with no other meds and normal labs? The risk is negligible.
Guidelines Clash: Who Says What?
There’s no global standard. Different groups give conflicting advice.
The British Thoracic Society (BTS) says: Everyone getting long-term macrolides (like for bronchiectasis or COPD) needs a baseline ECG. QTc over 450 ms in men or 470 ms in women? Don’t start the drug. Repeat the ECG after one month. This is strict, but it caught 1.2% of previously undiagnosed Long QT Syndrome cases.
The U.S. FDA and American Heart Association take a smarter approach: risk-based screening. They don’t demand ECGs for every patient. Instead, they use a 9-point scoring system that weighs age, sex, kidney function, and other meds. If you score 4 or higher? Get the ECG. If you’re low risk? Skip it.
And then there’s the real world. In UK respiratory clinics, 87% follow BTS rules. In U.S. primary care? Only 18% do. Why? Because most doctors aren’t trained to check QT intervals. And ECGs cost money-£28.50 per test in the UK. With 12 million macrolide prescriptions a year there, universal screening would cost £342 million. That’s not feasible.
What Happens If You Skip the ECG?
Most people finish their course without issue. But not all.
A Reddit post from March 2025 described a 68-year-old woman with a baseline QTc of 480 ms-borderline, but not flagged. She was given clarithromycin for pneumonia. Five days later, she went into Torsades de Pointes. Emergency cardioversion saved her life. Her ECG had been done months ago, but no one checked it before prescribing.
Another case: a 72-year-old man on azithromycin and furosemide. His potassium was low. His QTc was 510 ms. He collapsed at home. His family said he’d been “fine.” He didn’t survive.
These aren’t outliers. They’re predictable. And preventable.
How ECG Monitoring Actually Works in Practice
If you’re at risk, here’s what to expect:
- Before your first dose, your doctor orders a 12-lead ECG. It takes 5 minutes.
- The result is reviewed for QTc. Normal is under 450 ms for men, under 470 ms for women.
- If QTc is 450-499 ms? Your doctor may still prescribe the drug-but will monitor you closely. They’ll check your electrolytes, avoid other QT drugs, and schedule a follow-up ECG in 7-10 days.
- If QTc is 500 ms or higher? They’ll switch you to a safer antibiotic-like amoxicillin or doxycycline.
- For long-term users (like bronchiectasis patients), a repeat ECG at one month catches delayed prolongation.
Some clinics now use point-of-care devices that give QTc results in under a minute. One UK pilot cut the wait time for treatment from 5 days to less than a day. That’s a game-changer.

What Your Doctor Should Ask Before Prescribing
Don’t assume your doctor knows. Ask these questions:
- “Am I at risk for QT prolongation?”
- “Could this antibiotic interact with anything else I’m taking?”
- “Do you need to check my ECG before I start?”
- “What signs should I watch for-like dizziness, palpitations, or fainting?”
If your doctor says, “It’s fine,” and doesn’t ask about your meds, your age, or your heart history-that’s a red flag. Risk isn’t guesswork. It’s data.
The Future: Smarter Screening, Not More Tests
Health systems are catching on. By early 2025, 43% of U.S. hospitals using Epic EHR systems now get automated alerts when a macrolide is prescribed to someone with a high-risk profile. The system checks their age, sex, labs, and current meds-and flags the prescription if QT risk is elevated.
That’s the future: not universal ECGs for everyone, but smart alerts for the few who need them. It’s cheaper, faster, and saves lives.
Studies show that targeted screening reduces adverse events by 34%. In the U.S. alone, that could save $217 million a year-not by cutting care, but by cutting preventable emergencies.
Bottom Line: Don’t Ignore the Quiet Risks
Macrolides aren’t dangerous for everyone. But they’re not harmless either. The key is knowing who’s at risk-and acting on it.
If you’re over 65, female, on other meds, or have kidney issues: ask for an ECG before starting azithromycin or clarithromycin. If you’re young and healthy with no other drugs? The risk is tiny. But don’t assume. Ask.
One ECG, one question, one conversation-could be the difference between a routine antibiotic course and a cardiac emergency.


Jennifer Anderson
December 7, 2025 AT 22:28lol i just got azithromycin last week for my cough and no one even asked if i was on anything else. i take a multivitamin and that’s it. guess i’m lucky?
Helen Maples
December 9, 2025 AT 13:30There is no excuse for not checking QTc in patients over 65, especially women on diuretics. This isn't speculation-it's clinical negligence masked as convenience. The data is clear, the guidelines exist, and the cost of an ECG is negligible compared to the cost of resuscitating someone who coded because their provider skipped a five-minute test. Stop treating prevention like an optional luxury.
Olivia Hand
December 11, 2025 AT 09:18Someone needs to write a script that auto-pops up in EHRs when azithromycin is selected for anyone over 60 with any renal impairment or concurrent meds. Why is this still manual? We have algorithms for everything else-why not this? The tech exists. The risk is quantified. The inertia is the only thing killing people here.
Kyle Flores
December 12, 2025 AT 03:09I’m a nurse in a rural clinic and we don’t have an ECG machine on-site. We send people to the county hospital. Most won’t go unless they’re symptomatic. So we just avoid macrolides if they’re on any other meds or over 70. We use amoxicillin or doxycycline instead. It’s not perfect, but it’s safer than guessing.
Sadie Nastor
December 12, 2025 AT 22:22my grandma almost died from this and no one told us anything. she was on azithromycin for a chest cold and just… collapsed. they said it was "just bad luck." but she had kidney disease and was on a water pill. i wish someone had just asked one question. 🥺
Ted Rosenwasser
December 14, 2025 AT 15:56Let’s be real-this whole "risk stratification" is just a Band-Aid. The FDA’s 9-point scale is laughably inadequate. If you’re on a diuretic, over 65, and female, you’re already in the danger zone. Why not just screen everyone over 60? The marginal cost is pennies. The liability avoidance? Priceless. This isn’t medicine-it’s actuarial cowardice.
Nancy Carlsen
December 15, 2025 AT 15:51My aunt got an ECG before her azithromycin because she asked. Her QTc was 485. They switched her to amoxicillin and she’s fine now. It took 10 minutes. No one made her feel silly for asking. I wish more people knew they could-and should-ask.
David Brooks
December 15, 2025 AT 22:53THEY DIDN’T CHECK HER ECG. SHE WAS 72. SHE WAS ON FUROSEMIDE. HER QT WAS 510. SHE DIED. AND NOW HER FAMILY IS LEFT WITH A BURIAL BILL AND A QUESTION MARK THAT NEVER GOES AWAY. THIS ISN’T A "RARE" EVENT. IT’S A SYSTEM FAILURE. AND WE’RE ALL PAYING FOR IT IN GRIEF.
Ashley Farmer
December 17, 2025 AT 21:27Thank you for writing this. I work in a busy ER and I’ve seen too many of these cases. It’s heartbreaking because they’re all preventable. I wish more primary care docs would pause before hitting "prescribe." A quick look at meds, age, labs-takes 30 seconds. That’s all it takes to save a life.