When the temperature climbs above 30°C, most people think about drinking more water, staying in the shade, and avoiding the midday sun. But if you're taking diuretics or anticholinergics, those basic tips aren't enough. These medications can quietly turn a hot day into a medical emergency - even if you feel fine.
Why Diuretics Make Heat More Dangerous
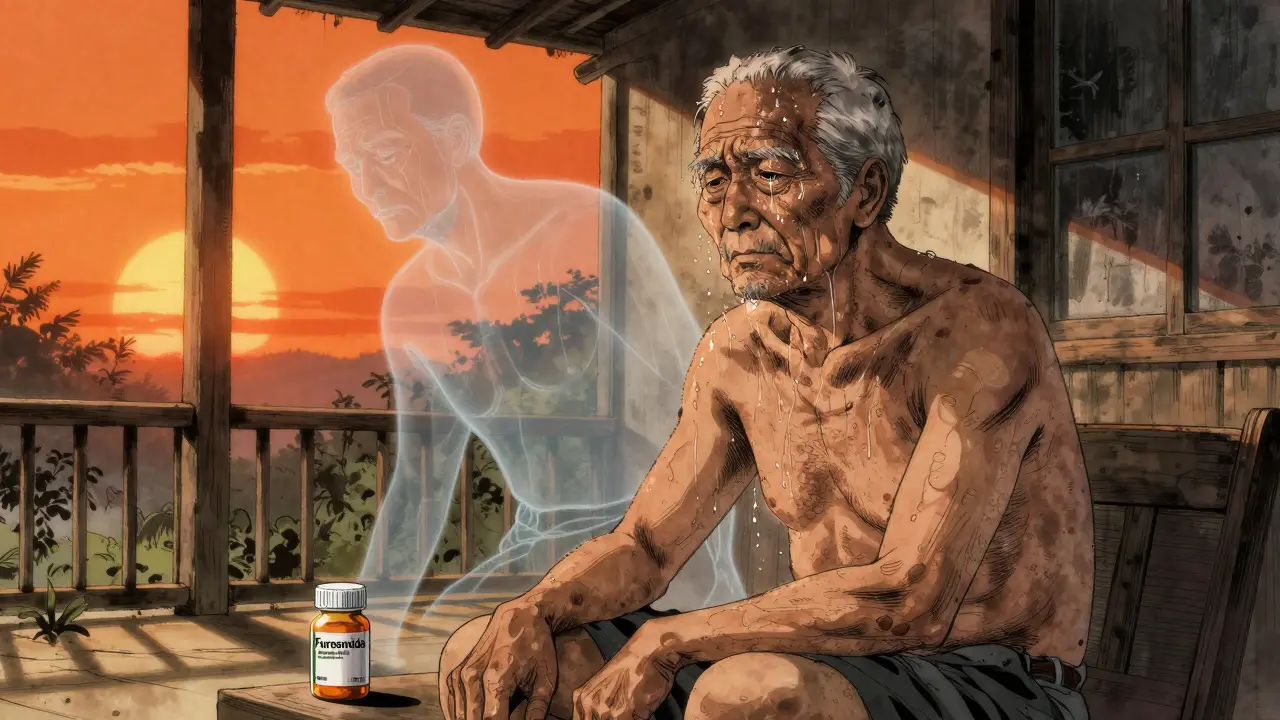
Diuretics - often called water pills - are prescribed to millions of people for high blood pressure and heart failure. Common ones include furosemide (Lasix), hydrochlorothiazide (HydroDiuril), and chlorthalidone (Hygroton). They work by helping your kidneys flush out extra fluid and salt. That’s good for your heart. But in hot weather, that same mechanism becomes a liability. Your body cools itself by sweating. Sweating needs fluid. Diuretics reduce your total fluid volume, making it harder for your body to produce enough sweat. In extreme heat, you can lose up to two liters of fluid per hour just from sweating. If you're on a diuretic, your body can't keep up. That leads to dehydration, low blood pressure, dizziness, and even fainting. Worse, many diuretics also cause potassium loss. Low potassium affects your heart rhythm. In heat stress, your heart is already working harder. Add low potassium, and you increase your risk of dangerous arrhythmias. A 2022 study of 1.2 million Medicare beneficiaries found that people on loop diuretics had a 37% higher chance of being hospitalized for heat-related illness - even when temperatures were only in the low 80s Fahrenheit (around 27°C). That’s not a heatwave. That’s a normal summer day in Adelaide.How Anticholinergics Block Your Body’s Cooling System
Anticholinergics are a different kind of threat. These drugs block acetylcholine, a chemical that tells your body to sweat. Common examples include oxybutynin (Ditropan) for overactive bladder, tolterodine (Detrol), and tricyclic antidepressants like amitriptyline. Here’s the scary part: if you're on a medication with a high anticholinergic burden (ACB score of 3), your body may sweat 30% to 50% less than normal. That’s not a small reduction. That’s like turning off your air conditioner in the middle of a heatwave. Your core temperature rises because your body can’t cool itself. Studies in the Journal of Thermal Biology showed that people on strong anticholinergics couldn’t regulate their core temperature during heat exposure - even if they were young and healthy. In older adults, this is even more dangerous. Many of these patients also have other conditions like dementia or Parkinson’s. Anticholinergics can make confusion worse. So when heat starts to affect them, they might not realize they’re in trouble. They don’t feel dizzy. They don’t say they’re hot. They just sit quietly. That’s how heat illness turns fatal.The Perfect Storm: When Medications Combine
The real danger isn’t just one medication. It’s the mix. Many older adults take multiple prescriptions. Someone might be on a diuretic for blood pressure, an anticholinergic for bladder control, and a beta-blocker for heart rhythm. Each one chips away at your body’s ability to handle heat. During the 2021 Pacific Northwest heat dome, over 90% of heat-related deaths involved people taking at least one medication that interfered with thermoregulation. Diuretics and anticholinergics were in 63% of those cases. This wasn’t random. It was predictable. And it’s happening again. In Australia, heat events are becoming more frequent and intense. Adelaide saw 17 days over 35°C in 2024 - the highest on record. If you’re on these medications, you’re not just at risk on extreme heat days. You’re at risk whenever the temperature rises above 26°C. That’s not a heat advisory. That’s Tuesday in January.What to Do: Practical Steps for Safety
You don’t have to stop your medication. But you do need to change how you manage your day in hot weather.- Drink more water - even if you’re told to limit fluids. If you have heart failure and your doctor told you to restrict water, talk to them before the heat hits. During extreme heat, fluid restrictions may need to be temporarily lifted. Your doctor can adjust this safely.
- Don’t wait until you’re thirsty. Thirst is a late sign of dehydration. Sip water consistently throughout the day. Keep a bottle with you. Set phone reminders if you need to.
- Wear loose, light-colored clothing. Dark clothes trap heat. Tight clothes trap sweat. Lightweight cotton lets what little sweat you produce evaporate - and that’s your only cooling tool if you’re on anticholinergics.
- Use sunscreen with SPF 30+. Many anticholinergics make your skin more sensitive to the sun. You can burn faster and more severely.
- Stay indoors between 11 a.m. and 4 p.m. Even air-conditioned homes aren’t enough. If your AC fails, go to a library, community center, or shopping mall. These places are cooling centers during heat events.
Recognize the Warning Signs - Before It’s Too Late
Heat illness doesn’t always start with a headache or nausea. Especially if you’re on anticholinergics, symptoms can be subtle - or absent. Watch for:- Unusual confusion or forgetfulness
- Dry skin (even if you’re sweating a little)
- Rapid heartbeat or palpitations
- Dark urine or very little urine
- Feeling unusually tired or weak
- Muscle cramps or twitching
Ask Your Doctor These Questions
Don’t assume your doctor knows you’re at risk. Bring this up before summer hits.- Is my medication known to affect sweating or fluid balance?
- Could my dose be adjusted during hot weather?
- Do I have other medications that might make this worse?
- What symptoms should I call you about?
- Who should I have check on me if I live alone?

Build a Safety Plan - Especially If You Live Alone
If you’re older, live alone, or have memory issues, you need a backup system. The CDC recommends a “buddy system.” That means one person checks on you at least twice a day during heat events. It could be a neighbor, a relative, a home care worker, or even a daily phone call from a community service. Make sure they know:- Your medication list
- What heat illness looks like in you
- When to call for help
What You Should Never Do
- Never stop your medication because you’re worried about heat. Stopping diuretics can cause dangerous fluid buildup. Stopping anticholinergics can cause sudden bladder or psychiatric symptoms. Always talk to your doctor first.
- Don’t rely on feeling fine. Anticholinergics can dull your awareness. You might not feel hot - even if your body is overheating.
- Avoid alcohol and caffeine. Both make dehydration worse. They’re not just bad choices - they’re dangerous when you’re on these meds.
The Bigger Picture
Climate change isn’t a future threat. It’s here. The number of days over 35°C in Adelaide has increased by nearly 50% since 1970. Heat-related deaths are rising. And medications like diuretics and anticholinergics are making it worse. Right now, most public health advice is generic: “Stay cool. Drink water.” But for people on these drugs, that’s not enough. We need personalized, medication-specific guidance. Until then, you have to be your own advocate. Know your meds. Know your risks. Know your plan. And don’t wait for a heatwave to start thinking about it.Can I still take my diuretic during a heatwave?
Yes - but you may need to adjust your fluid intake and possibly your dose. Never stop taking it without talking to your doctor. During extreme heat, fluid restrictions for heart failure patients may be temporarily lifted. Your doctor can help you find the right balance between managing your condition and staying safe in the heat.
Do anticholinergics stop me from sweating completely?
Not always - but they can reduce sweating by 30% to 50%, depending on the drug and dosage. Medications with a high anticholinergic burden score (ACB = 3), like oxybutynin or amitriptyline, have the strongest effect. Even small reductions in sweating can be dangerous in heat because your body loses its main way of cooling down.
Is it safe to use fans if I’m on these medications?
Fans help - but only if there’s some moisture on your skin to evaporate. If you’re on anticholinergics and barely sweating, a fan alone won’t cool you down. Combine it with cool water on your skin, a damp cloth on your neck, or a misting spray. Air conditioning is still the best option.
Can I replace my anticholinergic with a safer alternative?
Sometimes. For overactive bladder, newer options like mirabegron (Myrbetriq) don’t have anticholinergic effects. For depression, SSRIs like sertraline may be safer than amitriptyline. But switching isn’t always possible - and it must be done under medical supervision. Don’t change your meds on your own.
What should I do if I start feeling dizzy or confused in the heat?
Stop what you’re doing. Sit or lie down in a cool place. Drink water slowly. If you don’t feel better in 15-20 minutes, or if confusion gets worse, call emergency services. These symptoms could mean heat exhaustion or heat stroke - especially if you’re on diuretics or anticholinergics. Don’t wait. Heat illness can become life-threatening quickly.
Are children or younger adults at risk too?
Yes - but less commonly. Most people on these medications are older adults. However, younger people taking anticholinergics for conditions like severe allergies, Parkinson’s, or certain mental health disorders can still be at risk. Heat vulnerability isn’t about age - it’s about how the medication affects your body’s cooling system.
How do I know if my medication has a high anticholinergic burden?
Ask your pharmacist or doctor. Medications are scored on the Anticholinergic Cognitive Burden (ACB) scale. A score of 3 means strong effect - like oxybutynin, tolterodine, or amitriptyline. A score of 1 or 2 is lower risk. Many apps and online tools list ACB scores. Your pharmacist can check your full list and tell you which ones matter most.
Should I avoid outdoor exercise if I’m on these medications?
Yes - especially during peak heat hours. If you need to be active, do it early in the morning or late at night when it’s cooler. Keep it light: walking, stretching, or indoor yoga. Avoid intense workouts. Your body is already working harder to manage your condition - don’t add heat stress on top.

Retha Dungga
December 30, 2025 AT 21:15Jenny Salmingo
January 1, 2026 AT 20:35Aaron Bales
January 2, 2026 AT 13:57Lawver Stanton
January 2, 2026 AT 23:59Sara Stinnett
January 4, 2026 AT 12:25linda permata sari
January 5, 2026 AT 04:28Brandon Boyd
January 6, 2026 AT 16:38Branden Temew
January 8, 2026 AT 14:31