By 2025, the world will spend over $1.6 trillion on medicines. That’s more than the GDP of all but the top 15 economies. And yet, billions of people still pay for pills out of their own pockets - sometimes skipping doses because they can’t afford them. The key to keeping this system from collapsing isn’t more innovation. It’s generics.
Why Generics Are the Silent Backbone of Global Health
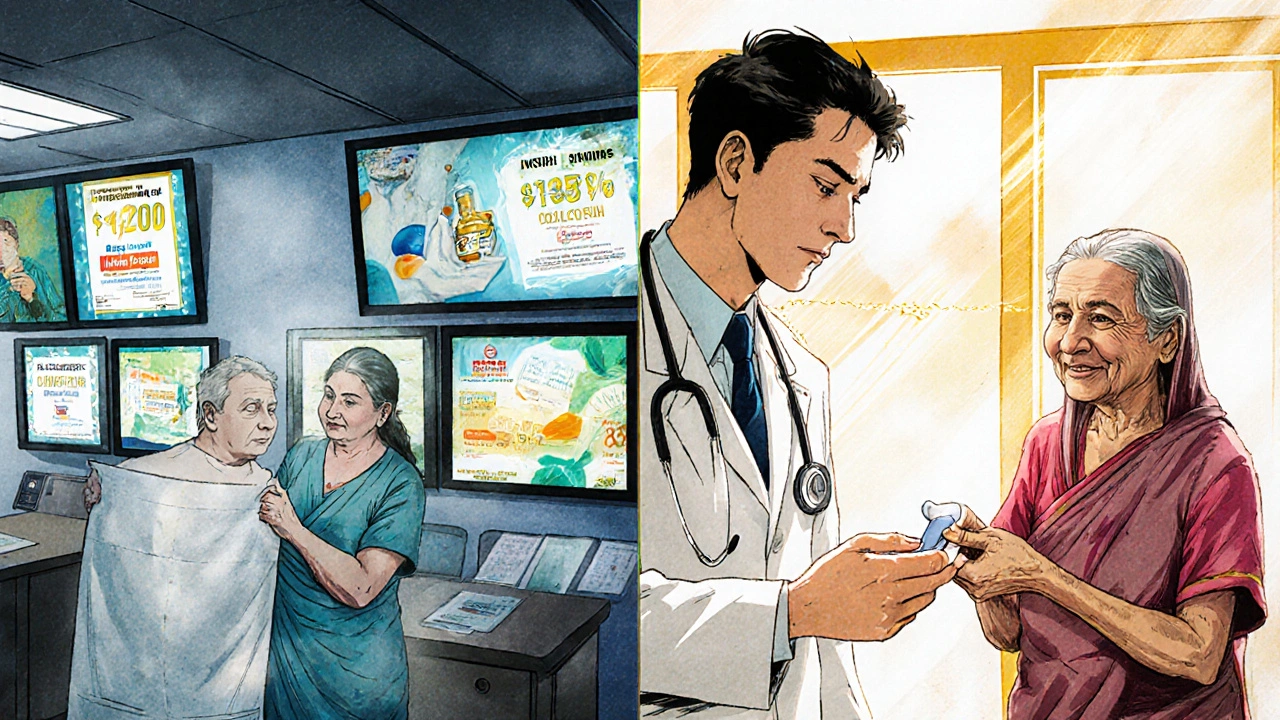
When you hear about breakthrough drugs that cost $1 million per patient, it’s easy to think that’s what healthcare looks like today. But in reality, 80 to 90% of all prescriptions filled in the U.S., Canada, and Western Europe are for generic drugs. These aren’t cheap knockoffs. They’re exact copies of brand-name medicines, approved by regulators, proven safe, and priced at 80-95% less.
In countries like India and Brazil, generics make up over 90% of the market. In Nigeria and Afghanistan, where most people pay for healthcare themselves, generics are often the only option. Without them, millions would go untreated. In 2022, 55 countries relied on out-of-pocket payments as their main source of health funding. In Turkmenistan and Armenia, people paid more than 75% of their healthcare bills directly. Generics didn’t just help - they made survival possible.
The U.S. Paradox: High Spending, High Prices, Low Savings
The United States spends more on healthcare than any other country - $5.6 trillion in 2025, and climbing to $8.6 trillion by 2033. Drug spending alone is projected to double from $776 billion to $1.7 trillion in that same timeframe. Yet, even here, generics are the only thing holding costs down.
In 2024, U.S. drug spending jumped $50 billion, mostly because of new, expensive treatments for obesity, diabetes, and cancer. But if you look at the actual prescriptions filled, over 90% were generics. The problem? The most expensive drugs - the ones that drive spending - are rarely generic. Oncology, immunology, and rare disease drugs are still under patent. And when they’re not, biosimilars (the generic version of biologic drugs) face regulatory delays, insurance resistance, and doctor hesitation.
Meanwhile, the average American pays $177 out of pocket for prescriptions in 2025. By 2033, that’s expected to hit $231. That’s a 30% increase. Generics could cut that number in half - if they were easier to access.
How the Rest of the World Is Doing It Differently
While the U.S. struggles with pricing battles, other regions are quietly getting smarter. In Europe, governments negotiate bulk prices and mandate generic substitution. In Germany, pharmacists can swap a brand-name drug for its generic version unless the doctor says no. In the U.K., the NHS has a formal list of preferred generics - and prescribers are monitored for cost efficiency.
In Latin America, countries like Colombia and Mexico have built national generic procurement programs. They buy in bulk, cut out middlemen, and pass savings to patients. Even in low-income countries, programs like the Global Fund and PEPFAR rely almost entirely on generics to treat HIV, TB, and malaria. These programs treat millions - and they do it for pennies on the dollar.
But it’s not all smooth sailing. In China, the market is shifting. As incomes rise, patients and doctors are demanding newer, branded drugs. Generics are no longer seen as just affordable - they’re seen as outdated. That’s a dangerous trend. If emerging economies follow this path without strong cost controls, their healthcare systems could collapse under the weight of innovation.
The Real Cost of Not Using Generics
When countries skip generics, they don’t just spend more - they spend unfairly. In 2022, high-income countries spent an average of 5.8% of their GDP on health. Upper-middle-income countries spent 4%. Lower-middle-income countries? 2.4%. Low-income countries? Just 1.2%. No low-income country met the World Health Organization’s recommended 5% benchmark.
And it’s getting worse. Between 2019 and 2021, 37 countries saw their real public health spending drop. Lebanon’s budget shrank by 71%. Malawi’s fell by 41%. In those places, generics aren’t a cost-saving tool - they’re the only thing keeping clinics open.
Meanwhile, global aid for health is falling. In 2025, it’s expected to drop to $39.1 billion - the lowest since 2009. That means countries can’t rely on outside help anymore. They have to make their own systems work. And that means choosing generics over expensive brands - even when it’s politically unpopular.
Why Biosimilars Are the Next Frontier
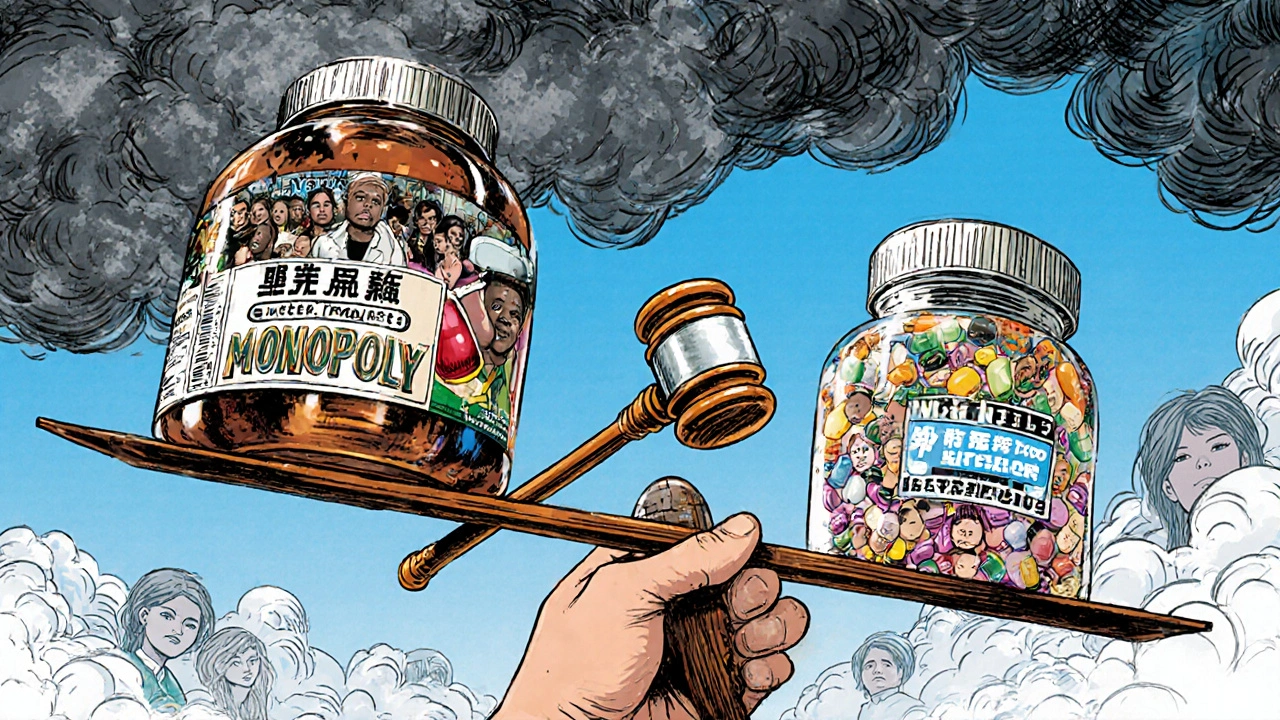
Biologic drugs - made from living cells - are the new frontier in medicine. They treat cancer, rheumatoid arthritis, and Crohn’s disease. But they’re also the most expensive. A single dose of a biologic can cost $10,000 a year. That’s why biosimilars - the generic version of these complex drugs - are so important.
But adoption is uneven. In the U.S., biosimilars make up less than 10% of the biologic market. Why? Insurance companies often don’t cover them. Doctors don’t know how to prescribe them. Patients are scared they won’t work as well. In Europe, biosimilar use is much higher - over 50% in some countries - because of clear policies and education.
The difference isn’t science. It’s policy. Countries that have clear rules for biosimilar approval, reimbursement, and physician training get better uptake. Those that don’t, leave patients paying more - and systems burning cash.
What’s Driving Up Costs - and What Generics Can’t Fix
It’s easy to blame drugs for rising healthcare costs. But the real drivers are bigger. Hospital care, specialist visits, and new medical technologies account for two-thirds of cost increases. In the Americas, 88% of insurers say new medical tech is the biggest cost driver. In Asia, it’s 73%.
Generics don’t fix hospital bills. They don’t lower the cost of MRIs or robotic surgery. But they do stop one part of the system from spiraling out of control. Without generics, drug spending would be 30-40% higher globally. That would push more people into medical poverty.
And here’s the kicker: medical costs are still rising. Globally, insurers expect a 10.4% average increase in 2025. In Asia Pacific, it’s 12.3%. In the Middle East and Africa, it’s 12.1%. Generics are the only tool we have that works everywhere - rich or poor, urban or rural, public or private.
The Future of Generics: More Than Just Cheap Pills
Generics aren’t just about price. They’re about access, equity, and sustainability. As more countries face aging populations, chronic disease spikes, and shrinking budgets, the choice isn’t between innovation and generics. It’s between innovation with generics - or innovation that breaks the system.
The next decade will see more patents expire. Dozens of blockbuster drugs will go generic. But only if governments act. They need to:
- Fast-track generic approval without compromising safety
- Require insurers to cover generics before brand-name drugs
- Train doctors to prescribe them confidently
- Stop letting patent thickets block competition
There’s no magic bullet. But generics are the closest thing we have.
Are generic drugs as safe as brand-name drugs?
Yes. Generic drugs must meet the same strict standards as brand-name drugs. Regulators like the FDA, EMA, and WHO require generics to have the same active ingredient, strength, dosage form, and route of administration. They must also prove they’re absorbed into the body at the same rate and extent. The only differences are in inactive ingredients - like fillers or dyes - which don’t affect how the drug works. Millions of people take generics every day without issue.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials. They rely on the original drug’s safety and efficacy data, which has already been approved. That cuts development costs by 80-90%. They also face competition from multiple makers once a patent expires, which drives prices down further. A single generic drug can have 10-20 manufacturers competing to sell it, while brand-name drugs often have no competition.
Do generics work as well for chronic conditions like high blood pressure or diabetes?
Absolutely. For decades, generics have been the standard for treating chronic conditions. In the U.S., over 90% of prescriptions for blood pressure meds, statins, and metformin are generics. Studies show no difference in outcomes between brand and generic versions. Patients who switch from brand to generic for hypertension or diabetes see the same control of their condition - and pay a fraction of the cost.
Why aren’t biosimilars used more widely in the U.S.?
It’s not about effectiveness - it’s about money and bureaucracy. Biologics are complex and expensive to produce, so biosimilars are harder to make. But the bigger issue is that drugmakers pay insurers and pharmacy benefit managers to block biosimilars. They offer rebates to keep brand-name drugs on preferred lists. Doctors aren’t always trained to prescribe them. And patients are often told, "This one’s better," even when there’s no evidence. In Europe, government policies force substitution and education - so adoption is much higher.
Can countries with low healthcare budgets afford to skip generics?
No - and many already can’t. In low-income countries, spending on health averages just 1.2% of GDP. Generics are the only reason millions with HIV, TB, or malaria can get treatment. Without them, global health programs would need 5-10 times more funding. Countries like Malawi and Afghanistan rely on generics for 95% of their medicine supply. Skipping them isn’t an option - it’s a death sentence for public health.


Bartholemy Tuite
November 24, 2025 AT 15:45man i lived in dublin for a year and saw how the nhs just swaps generics like its nothing and people dont even notice the difference in pills
here in the states its like we pay for the brand name logo not the medicine
my grandma takes metformin and her script was $400 for the brand then $3 for the generic
she cried when she found out she was getting scammed for years
its not rocket science
same active ingredient same results
but the pharma lobby has us all brainwashed into thinking expensive = better
its a scam dressed up as science
and dont get me started on how they pay insurers to block biosimilars
the whole system is rigged
and yet we act surprised when people skip doses
its not that theyre lazy its that theyre broke
and the worst part
we all know this
but we keep voting for the same people who let it happen
Nikki C
November 25, 2025 AT 06:49generics are the unsung heroes of global health
no one throws parades for them
but they keep millions alive
and the fact that we still treat them like second class meds is insane
in india my cousin gets her blood pressure pills for 20 cents a month
here i paid $120 for the same thing last year
its not about quality
its about power
and the people who profit from this arent doctors
theyre executives in boardrooms
and we let them
Alex Dubrovin
November 27, 2025 AT 01:51my dad had cancer
he was on a biologic
cost $15k a month
insurance denied it twice
we had to sell the truck
then a biosimilar came out
same thing
cost $3k
insurance approved in a week
he lived 3 more years
because someone finally made the switch
stop acting like generics are a compromise
theyre the solution
Akash Chopda
November 28, 2025 AT 11:30generics are a government plot to control the population
the same people who push generics also push vaccines
and mandating substitution
its all connected
they want you dependent on cheap pills
so you dont ask questions
look at india
they export generics
but their own people are dying of malnutrition
its not about health
its about control
theyre replacing real medicine with factory pills
and you guys are cheering
Jacob McConaghy
November 30, 2025 AT 02:04the real tragedy is that we have the solution
but we dont use it
generics are cheaper
safer
just as effective
and yet doctors still write brand names
because theyre told to
because reps give them free lunches
because the system rewards volume not value
we dont need new drugs
we need better systems
we need pharmacists to swap without asking
we need insurance to cover generics first
we need patients to demand it
but instead we just pay and shut up
thats not healthcare
thats surrender
Natashia Luu
December 1, 2025 AT 23:33How dare you suggest that generics are acceptable for chronic conditions? The FDA’s own data shows that 12% of patients report adverse effects when switching from brand to generic. This is not a cost-saving measure-it is a public health catastrophe waiting to happen. The pharmaceutical industry invests billions in research, and to devalue their work by promoting inferior alternatives is not only irresponsible-it is morally indefensible. We must protect innovation, not sacrifice it for convenience.
Vineeta Puri
December 3, 2025 AT 11:48As someone who works in public health in rural India, I can say with certainty that generics are the foundation of survival here
we don’t have luxury
we have need
and generics meet that need with dignity
patients don’t care about the label
they care about breathing
about seeing their children grow
about not dying because a pill cost too much
when we talk about equity
this is what it looks like
not in boardrooms
but in village clinics
where a $0.10 pill keeps a mother alive
and that is worth more than any patent
Victoria Stanley
December 3, 2025 AT 23:29just wanted to add that biosimilars are actually way more straightforward than people think
they go through the same rigorous testing
the only difference is the manufacturing process
but the outcome? identical
in the u.s. we have this weird fear of anything that’s not branded
like if it’s cheaper it must be weaker
but that’s not science
that’s marketing
and honestly
it’s hurting people
my uncle switched to a biosimilar for rheumatoid arthritis
saved $12k a year
same results
same side effects
same quality
why are we still making this a moral issue?
it’s just medicine
Andy Louis-Charles
December 4, 2025 AT 11:26generics are life
period
if you’ve never had to choose between rent and insulin
you don’t get to judge
the fact that we even have to argue about this
is a national shame
and biosimilars? they’re the future
but only if we stop letting big pharma buy politicians
and start letting pharmacists do their job
👍
Douglas cardoza
December 5, 2025 AT 16:08my pharmacy gives me the generic automatically
and i never knew until last year that my blood pressure med was branded before
no difference
same pills
same results
just cheaper
why is this even a thing
we’re literally paying extra for packaging
and a logo
and i feel like i’m the only one who thinks that’s insane
Adam Hainsfurther
December 6, 2025 AT 22:20the real question is why aren’t we pushing for mandatory generic substitution everywhere
not just in europe
but in every country
if it’s safe
if it’s effective
why is the choice even up to the doctor
why should a patient’s income determine what medicine they get
the system is built to profit from suffering
and we’re all just playing along
until it’s our turn
to skip doses
to sell things
to beg for help
Rachael Gallagher
December 7, 2025 AT 13:12generics are for losers who can’t afford real medicine
if you’re poor
that’s your fault
not the system’s
and if you want to live
you should work harder
not beg for cheap pills
we’re not a third world country
we have the best tech
the best drugs
and we should use them
no matter the cost
because we’re worth it