Oral Anesthesia Agent Selector
Select an anesthetic and click "Analyze Agent Properties" to see detailed information.
| Agent | Onset Time | Duration | Max Dose |
|---|---|---|---|
| Lidocaine | 2-4 minutes | 1-3 hours | 300 mg |
| Articaine | 1-3 minutes | 1-2 hours | 500 mg |
| Mepivacaine | 3-5 minutes | 1-2 hours | 400 mg |
When you sit in the dentist’s chair and feel that familiar pinch before the drill starts, you’re witnessing a well‑orchestrated chemical process that temporarily blocks pain signals. Understanding local anesthesia helps you feel more in control, reduces anxiety, and lets you follow your dentist’s instructions with confidence.
Quick Takeaways
- Local anesthesia works by interrupting nerve signal transmission at the site of injection.
- Lidocaine, articaine, and mepivacaine are the most common agents, each with distinct onset and duration.
- A typical oral cavity procedure follows a five‑step workflow: assessment, preparation, injection, waiting for numbness, and treatment.
- Side effects are rare but can include temporary tingling, bruising, or, in very rare cases, allergic reactions.
- Following simple pre‑ and post‑procedure tips speeds recovery and minimizes discomfort.
What Is Local Anesthesia in the Mouth?
Local anesthesia in oral cavity procedures is a temporary loss of sensation achieved by injecting a medication directly into the tissues surrounding a tooth or gum. The medication blocks the nerves that carry pain signals to the brain, allowing the dentist to work without the patient feeling sharp or throbbing sensations. Unlike general anesthesia, you stay fully awake, can breathe normally, and recover instantly once the drug wears off.
How the Nerve Block Actually Stops Pain
The gut feeling that a needle will “numb” you is more than a metaphor-there’s a clear biophysical pathway.
- Targeting the nerve fibers: Every tooth is surrounded by a network of sensory nerves (the superior and inferior alveolar nerves for upper and lower teeth). The dentist positions the needle close to these fibers.
- Drug diffusion: Once injected, the anesthetic molecule diffuses across the neuronal membrane and enters the nerve’s interior.
- Blocking sodium channels: The key action is the reversible binding to voltage‑gated sodium channels. Sodium channels are responsible for the rapid rise of electrical charge that creates a nerve impulse. When they’re blocked, the impulse can’t travel.
- Interrupting signal transmission: With the channels shut, the pain signal never reaches the spinal cord, and consequently, the brain never registers it.
- Reversal: As the drug is metabolized or absorbed into the bloodstream, the channels reopen and normal sensation returns.
This mechanism is the same for any peripheral nerve block, but the oral cavity presents unique challenges: limited space, proximity to vital structures, and the need for precise depth control.
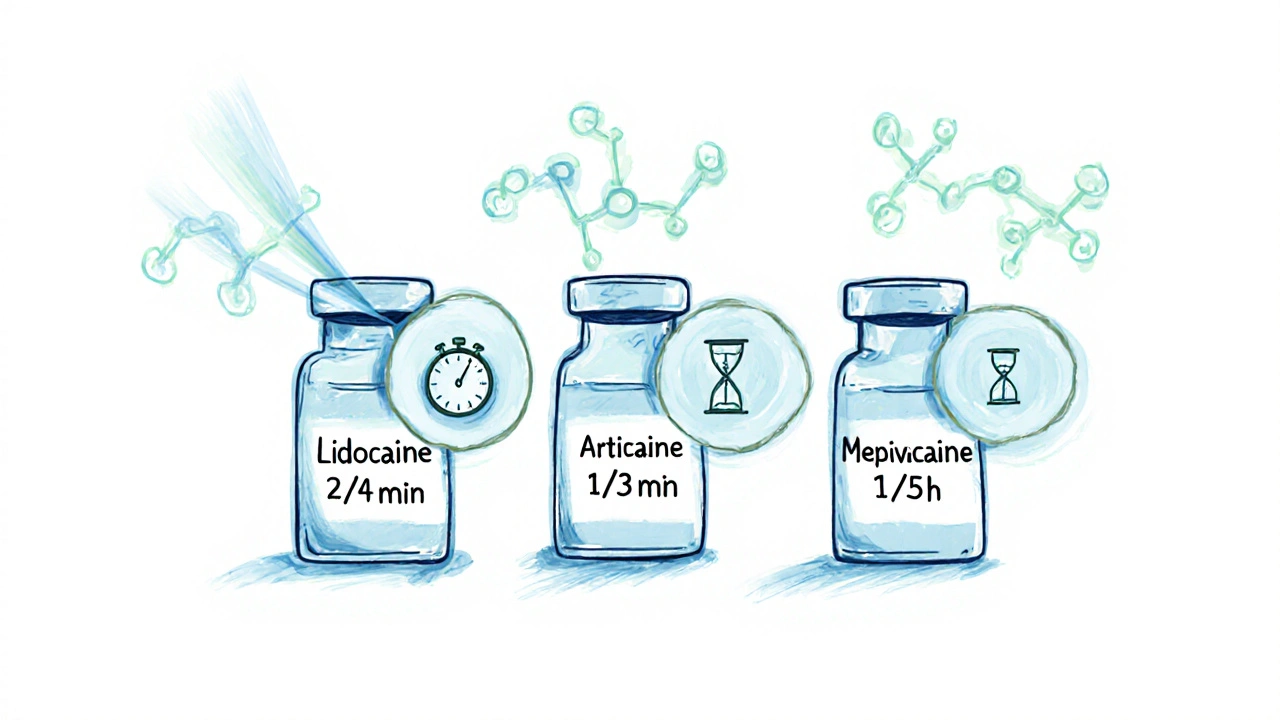
Common Local Anesthetic Agents Used in Dentistry
Dental professionals choose the anesthetic based on how quickly it works, how long it lasts, and the patient’s health profile. Below is a snapshot of the three most frequently used agents.
| Agent | Typical Onset | Duration of Numbness | Maximum Single Dose (mg) |
|---|---|---|---|
| Lidocaine | 2-4 minutes | 1-3 hours | 300 (without epinephrine) |
| Articaine | 1-3 minutes | 1-2 hours | 500 (with 1:100,000 epinephrine) |
| Mepivacaine | 3-5 minutes | 1-2 hours | 400 (without epinephrine) |
All three agents are often combined with a vasoconstrictor such as epinephrine (1:100,000 or 1:200,000). The vasoconstrictor narrows blood vessels, slowing the drug’s absorption so the numbness lasts longer and bleeding is reduced.
Step‑by‑Step: What Happens During an Oral Cavity Procedure
Knowing the exact flow of a typical appointment helps you stay relaxed. Here’s what most dentists follow:
- Initial assessment: The dentist reviews your dental history, asks about allergies (especially to anesthetic agents), and selects the appropriate drug.
- Preparation of the site: The gum is cleaned with an antiseptic swab. A topical anesthetic gel may be applied for a few seconds to soften the skin’s surface.
- Injection technique: Using a thin, beveled needle (27‑30 gauge), the clinician injects the anesthetic near the targeted nerve. Common techniques include:
- Inferior alveolar nerve block (lower teeth)
- Posterior superior alveolar block (upper molars)
- Infiltration (single tooth or small area)
- Waiting for numbness: Depending on the agent, the dentist waits 2‑5 minutes. They may gently poke the tissue to confirm loss of sensation.
- Performing the procedure: With the area numb, the dentist carries out fillings, extractions, crowns, or gum surgery. Because you’re still conscious, you can follow instructions like “bite down gently” if needed.
- Post‑procedure check: Once the work is done, the dentist may rinse the area, give after‑care instructions, and note when the numbness is expected to fade.
Even though the steps are straightforward, each step carries its own nuances that affect comfort and safety.
Safety, Side Effects, and What to Watch For
Local anesthetics are among the safest drugs used in dentistry, but a few considerations are worth noting.
- Allergic reactions: True allergies to amide‑type anesthetics (lidocaine, articaine) are rare (<0.1%). If you have a known allergy, inform the dentist; alternative agents like prilocaine may be used.
- Systemic toxicity: Over‑dosing can cause dizziness, ringing in the ears, or, in extreme cases, seizures. Dentists calculate the dose based on body weight and avoid injecting near highly vascular areas without a vasoconstrictor.
- Localized complications: Bruising, swelling, or a brief “pins‑and‑needles” sensation are normal and resolve within a few hours. Persistent numbness beyond 24hours warrants a call to the clinic.
- Interaction with medications: Certain heart medications (beta‑blockers) and monoamine oxidase inhibitors can heighten effects of epinephrine. Always list your current drugs.
By adhering to dosage guidelines and monitoring the injection site, dentists keep risks to a bare minimum.

Patient Tips: Before, During, and After the Numbing
Small habits can make the whole experience smoother.
Before the appointment
- Eat a light meal - an empty stomach can make you feel faint when the vasoconstrictor raises blood pressure.
- Avoid caffeine and nicotine for a few hours; they can constrict blood vessels and affect how the anesthetic spreads.
- Discuss any recent illnesses, infections, or medication changes with your dentist.
During the injection
- Practice slow, deep breathing. Focusing on your breath reduces the perception of the needle’s pressure.
- If the dentist asks you to “bite down,” do so gently on a cotton roll to protect soft tissues while the anesthetic works.
After the procedure
- Don’t eat until the numbness fully fades - you could bite your cheek, tongue, or lip.
- Keep the area clean with a gentle salt‑water rinse (½tsp salt in 8oz warm water) after the first 24hours.
- If you experience prolonged swelling, throbbing pain, or a metallic taste, contact the dental office promptly.
When to Seek Professional Help
Most post‑procedure sensations are temporary, but some signs call for immediate attention:
- Severe, spreading swelling that doesn’t subside after 48hours.
- Sharp, burning pain that intensifies rather than eases.
- Fever above 38°C (100.4°F) indicating possible infection.
- Loss of feeling that lasts more than 24hours without improvement.
Prompt communication with your dental team helps prevent complications and ensures quick recovery.
Frequently Asked Questions
How long does the numbing effect last?
Most single‑tooth infiltrations with lidocaine wear off in 1-3hours. Nerve blocks for larger areas may last up to 4hours, depending on the vasoconstrictor used.
Can I be allergic to lidocaine?
True allergic reactions to lidocaine are extremely rare. Most reported “allergies” are actually sensitivities to the preservative (methylparaben) or to a vasoconstrictor. Your dentist will ask about any prior reactions before choosing an agent.
Is it safe to have multiple teeth anesthetized in one visit?
Yes, as long as the total dose stays within the recommended maximum based on your weight. Dentists calculate the amount carefully and may spread the injections over a short period to stay within safe limits.
Why does my lip feel tingly after a root canal?
The tingling is a normal sign that the anesthetic is still active. The nerves that serve the lip share pathways with the dental nerves, so they may stay numb a little longer. The feeling fades as the drug metabolizes.
Can I drive home after receiving local anesthesia?
Absolutely. Since you remain fully conscious and your cognitive functions are unchanged, driving is safe. If a vasoconstrictor was used, you might feel a mild increase in heart rate, but it does not impair driving ability.


Randy Faulk
October 5, 2025 AT 14:39In dental anesthesia, lidocaine and its counterparts act as reversible antagonists of voltage‑gated sodium channels, thereby halting the rapid depolarization necessary for nociceptive transmission. By diffusing across the neuronal membrane, the molecule binds intracellularly, stabilizing the inactivated state of the channel. This prevents the influx of Na⁺ ions, which is essential for the generation of an action potential. Consequently, the pain signal is arrested at its source, leaving the patient insensate for the duration of the drug’s presence.
Brandi Hagen
October 13, 2025 AT 03:13Let me break down the entire saga of local anesthesia like it’s a blockbuster thriller 🎬. First, the dentist chooses the hero of the story – lidocaine, articaine, or mepivacaine – each with its own origin story and secret powers. 🎭 Then, the tiny needle, that stealthy infiltrator, sneaks past the gum’s defenses like a master spy, delivering the anesthetic directly to the nerve’s doorstep. 🚀 The drug spreads, not unlike a virus in a sci‑fi plot, hijacking sodium channels and declaring a state of emergency that blocks pain signals. 🌌 As the sodium channels shut down, the patient experiences that surreal “numb” sensation, a feeling akin to being stuck in a dream where you can’t feel a single poke. 😴 The wait time? A suspenseful pause of a few minutes, building tension before the grand reveal of complete numbness. 📈 Once the procedure starts, the dentist works with the confidence of a seasoned director calling “action!” while the patient sits there, blissfully unaware, like a moviegoer engrossed in the climax. 🎥 After the climax, the drug’s effect wanes, the sodium channels reopen, and sensation returns like the final credits rolling. 🎞️ The entire episode, from selection to recovery, is a tightly edited sequence of biochemical wizardry, precise technique, and patient trust. For those who think it’s just a simple “pinch”, this is a high‑octane drama where every minute counts and science steals the show! 🌟
isabel zurutuza
October 20, 2025 AT 15:46Wow another "educational" post about teeth numbness how original this is its not like we see these words everywhere lol
James Madrid
October 28, 2025 AT 03:19Great breakdown, Randy! Your step‑by‑step on sodium channel blockade really clarifies why we feel nothing during the procedure. I’ve always found the biochemistry a bit intimidating, but your explanation makes it feel approachable. Keep the science coming!
Justin Valois
November 4, 2025 AT 15:53Yo Brandi, that drama was over the top but hey good job 🤷♂️. Lemme add that articaine is actually the real MVP in deep jaw work, it penetrates like a ninja. Also, the vasoconstrictor is not just for bleedin, it slows absorption, so the numb lasts longer. If u want a quick fix for a molar, go with articaine plus epi. The only con? Some peeps get a weird tingling, but it’s nothing serious.
Jessica Simpson
November 12, 2025 AT 04:26From a cultural perspective, it’s interesting how different countries prefer certain agents. In Canada, many clinicians lean toward lidocaine with epinephrine for its well‑documented safety profile, while in parts of Europe articaine has become the standard for molar extractions. This variation often reflects local training curricula and regulatory approvals.
Ryan Smith
November 19, 2025 AT 16:59Sure, the “science” is sound, but have you ever wondered why the big pharma pushes these anesthetics? Something about controlling pain perception that could be useful for… other agendas. Just a thought.
John Carruth
November 27, 2025 AT 05:33I love how thorough this guide is-especially the part about waiting for numbness before proceeding. It’s so easy to rush, but taking those extra minutes can make the difference between a smooth experience and a patient’s panic. Also, the tip on using a topical gel first really helps the needle insertion feel less like a surprise attack. Keep sharing these nuggets of wisdom; they empower both patients and new dentists alike.
Melodi Young
December 4, 2025 AT 18:06Honestly, it’s just basic stuff.
Tanna Dunlap
December 12, 2025 AT 06:39While the guide is informative, it glosses over the ethical responsibility of ensuring informed consent. Patients should be fully aware of potential side effects, however rare, before any injection. Ignoring this can erode trust in the profession.
Troy Freund
December 19, 2025 AT 19:13James made a solid point about the sodium channel mechanism; it’s a reminder that every tiny chemical interaction carries philosophical weight-our perception of pain is just a cascade of ions, and with the right knowledge we can alter that reality. Fascinating, isn’t it?
Mauricio Banvard
December 27, 2025 AT 07:46Did you know that the “safe” dosage limits are based on studies funded by manufacturers? Some independent researchers suggest those numbers might be conservative, yet others claim they’re overly generous. It’s a murky world out there.
Paul Hughes
January 3, 2026 AT 20:19Nice summary! 😊 This will definitely help anyone nervous about their next dental visit.
Mary Latham
January 11, 2026 AT 08:53i think lidocaine is overrated its not the best they always push it because its a classic but articaine does the job faster lol
Marie Green
January 18, 2026 AT 21:26Reading this, I felt a wave of reassurance. Knowing exactly what’s happening can calm nerves, especially for those with dental anxiety. Thanks for the clear guide.
TOM PAUL
January 26, 2026 AT 09:59Hey folks, stay motivated! Understanding the science behind local anesthesia empowers you to ask the right questions and feel confident during procedures. You’ve got this!
Ash Charles
February 2, 2026 AT 22:33Great info! If you’re nervous, remember the needle’s tiny and the effect wears off fast. Trust the dentist’s skill.
Michael GOUFIER
February 10, 2026 AT 11:06Esteemed readers, the present exposition elucidates the pharmacodynamic principles governing local anesthetic administration within the oral cavity. It is incumbent upon practitioners to assimilate such knowledge to uphold the highest standards of patient care.
michael Mc Laughlin
February 17, 2026 AT 23:39Sounds good. Good luck with your next dentist visit.
Luke Schoknceht
February 25, 2026 AT 12:13Your guide is thorough, yet it fails to address the subtle yet critical issue of cumulative dosage in patients receiving multiple procedures in a single session. Overlooking this can lead to systemic toxicity, especially in vulnerable populations. Moreover, the description of vasoconstrictor use omits a discussion on contraindications in hypertensive patients, which is a glaring oversight. The lack of commentary on alternative non‑pharmacologic pain management techniques-such as hypnosis or guided imagery-also limits the scope of the article. While the tables are helpful, a visual flowchart could enhance comprehension for lay readers. Finally, the narrative could benefit from more patient‑centered language, emphasizing comfort and empowerment rather than a purely clinical perspective.