HLA-B*57:01 Test Interpreter
How This Tool Works
This tool helps clinicians interpret HLA-B*57:01 test results to guide abacavir treatment decisions in HIV patients. Based on CDC and FDA recommendations, patients testing positive for HLA-B*57:01 should avoid abacavir to prevent severe hypersensitivity reactions.
HLA-B*57:01 Test Result
Quick Takeaways
- Testing for HLA‑B*57:01 before starting abacavir cuts hypersensitivity risk by >95%.
- Pharmacogenetics links a patient’s DNA to drug safety and efficacy.
- CDC and FDA recommend genotyping as standard of care for abacavir.
- When the test is negative, abacavir remains a cost‑effective option for many HIV patients.
- Future panels may combine HLA testing with broader antiretroviral genomic profiles.
Imagine being able to skip a life‑threatening reaction simply by looking at a swab of blood. That’s the promise of pharmacogenetics in modern HIV care. This article walks through why a single genetic marker, HLA‑B*57:01, dictates whether a patient should receive Abacavir is a nucleoside reverse transcriptase inhibitor (NRTI) used in combination antiretroviral therapy for HIV infection, and how clinicians turn that knowledge into safer prescribing.
What Is Pharmacogenetics?
Pharmacogenetics is the study of how genetic variations influence an individual’s response to medications. It sits at the crossroads of genetics, pharmacology, and clinical medicine. By identifying DNA differences that affect drug metabolism, transport, or target interaction, doctors can predict who will benefit, who may need a dose tweak, and who should avoid a drug altogether.
The field exploded after the Human Genome Project gave researchers a catalog of common variants. Today, point‑of‑care genotyping kits and electronic health record alerts make it possible to apply this science in everyday clinics.
Why Abacavir Needs a Genetic Lens
Abacavir works by mimicking the natural building block guanosine, getting incorporated into viral DNA and causing premature chain termination. It’s a backbone of many first‑line regimens because it’s potent, cheap, and generally well‑tolerated.
However, about 5-8% of patients develop a severe hypersensitivity reaction (HSR) within the first six weeks. The reaction can involve fever, rash, gastrointestinal distress, and in rare cases, airway obstruction or shock. The culprit? A specific immune response linked to the HLA‑B*57:01 allele.
HLA‑B*57:01 and the Hypersensitivity Puzzle
The human leukocyte antigen (HLA) system presents peptide fragments to T‑cells. Certain drugs, like abacavir, bind directly to the HLA‑B*57:01 pocket, altering the repertoire of peptides displayed. In carriers, this triggers an unwanted immune cascade-what we call abacavir‑hypersensitivity syndrome.
Large prospective studies, including the PREDICT‑1 trial, showed that carriers of HLA‑B*57:01 have a >90% chance of developing HSR if given abacavir, while non‑carriers virtually never experience it. This stark contrast makes the allele a perfect predictive biomarker.
Guidelines and Regulatory Stance
The FDA mandates labeling that recommends HLA‑B*57:01 testing before abacavir initiation. Likewise, the CDC issues clinical recommendations that genotyping be performed as a standard of care for all patients starting abacavir. Both agencies cite evidence that pre‑emptive testing prevents costly hospitalizations and improves overall treatment adherence.
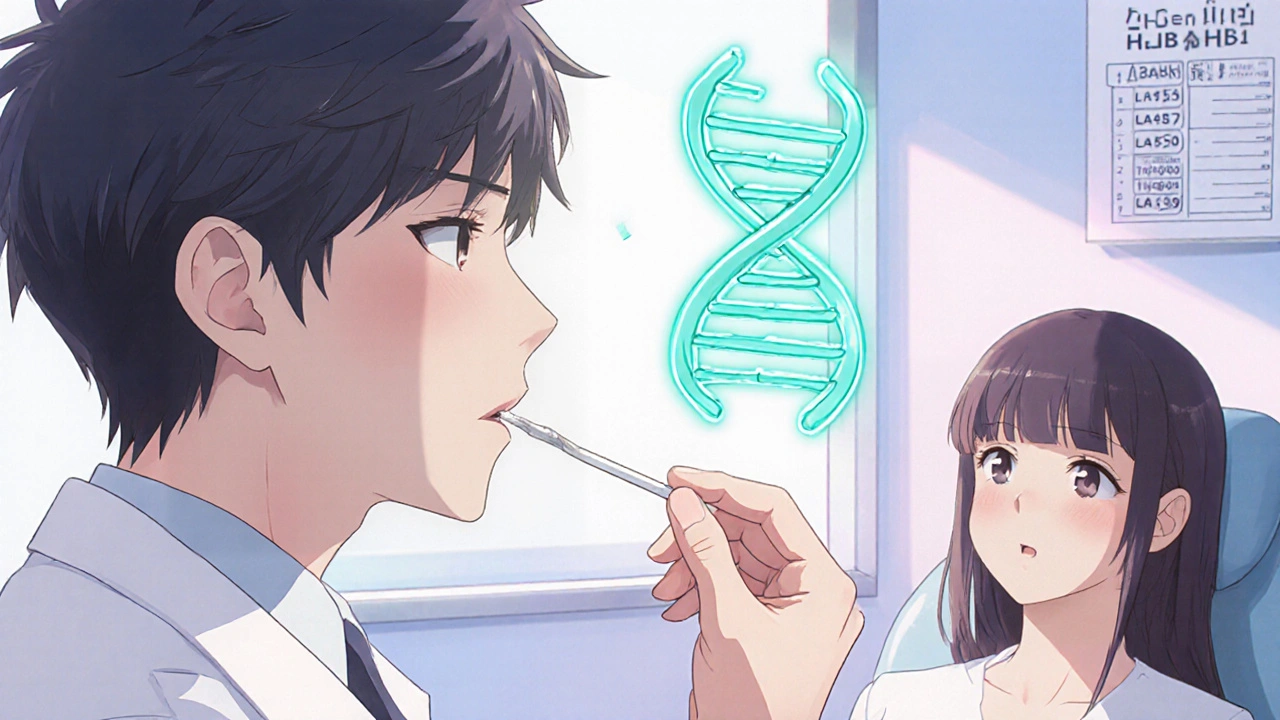
In practice, the workflow looks like this:
- Order a commercial HLA‑B*57:01 genotyping test (blood or buccal swab).
- Receive results within 24-72 hours from most labs.
- If negative, proceed with abacavir; if positive, choose an alternative NRTI (e.g., tenofovir).
Clinical Decision‑Making: From Test to Prescription
When the result is negative, clinicians gain confidence to prescribe abacavir, especially for patients who need a nucleoside backbone with a favorable lipid profile. The drug’s low impact on renal function makes it attractive for aging HIV populations.
If the test returns positive, the alternative options include tenofovir alafenamide (TAF) or lamivudine, depending on resistance patterns and comorbidities. The key is that the decision is now driven by hard data, not trial‑and‑error.
Electronic health records often embed alerts: “HLA‑B*57:01 positive - do not prescribe abacavir.” This reduces prescribing errors, especially in busy outpatient settings.
Benefits of a Pharmacogenetic Approach
- Patient safety: >95% reduction in HSR incidence.
- Cost savings: Avoided hospital stays offset the modest price of genotyping (≈ AU$50 in Australia).
- Adherence gains: Fewer adverse events translate to higher rates of viral suppression.
- Personalized care: Patients feel heard when their genetic profile guides therapy.
Challenges and the Road Ahead
Even with clear guidelines, implementation gaps exist. Rural clinics may lack rapid testing logistics, and insurance coverage can vary. Moreover, ethnicity influences allele prevalence-up to 15% in European ancestry, <1% in East Asian groups-so blanket policies may miss high‑risk subpopulations.
Research is expanding beyond HLA‑B*57:01. Multi‑gene panels now include CYP2B6 (affecting efavirenz metabolism) and CCR5 Δ32 (influencing entry inhibitor response). In the next decade, clinicians may order a single “HIV pharmacogenome” test that covers dozens of drug‑gene pairs.
Finally, education remains vital. Physicians, pharmacists, and patients must understand why a simple swab can change a treatment plan.
Quick Checklist for Starting Abacavir
- Order HLA‑B*57:01 genotyping before the first dose.
- Review results: negative → proceed; positive → select alternative NRTI.
- Document genotype in the patient’s medical record.
- Educate the patient about potential signs of hypersensitivity, even after a negative test (rare false‑negatives).
- Re‑evaluate if the patient starts a new medication that may interact with abacavir’s metabolism.
Frequently Asked Questions
Is HLA‑B*57:01 testing required for everyone?
Yes. Both the FDA and CDC consider it standard of care because the test is quick, inexpensive, and prevents a potentially fatal reaction.
How long does the genotyping result take?
Most commercial labs return results within 24-72 hours. Some point‑of‑care platforms can deliver results in under an hour.
What if a patient tests positive but still needs abacavir?
Current guidelines advise against abacavir in carriers. Alternatives like tenofovir or lamivudine are equally effective and safer.
Does the test work for children and infants?
Yes. The assay works on small blood volumes or buccal swabs, making it suitable for pediatric patients.
Are there any false‑negative results?
False‑negatives are extremely rare (<0.5%). However, clinicians should still monitor for any early signs of hypersensitivity during the first weeks of therapy.
Comparison: Genotyping vs. No Genotyping
| Scenario | Risk of HSR | Clinical Action |
|---|---|---|
| Genotype negative | ~0.1% | Start abacavir safely |
| Genotype positive | ~90% if given abacavir | Choose alternative NRTI |
| No genotype | 5-8% overall | Rely on clinical monitoring only |
Seeing the numbers side by side makes it clear: a simple genetic test reshapes risk from a handful of percent to almost zero for the right patients. That’s the power of pharmacogenetics.

Ashok Kumar
October 21, 2025 AT 17:25Wow, another excuse to brag about fancy DNA tests, huh? I get it, saving a few lives is nice, but the paperwork feels endless. Still, if a quick swab can stop a nasty reaction, why not?
Jasmina Redzepovic
October 26, 2025 AT 07:32Let me be clear: the United States has been at the forefront of integrating HLA‑B*57:01 genotyping into standard treatment algorithms, and the CDC-FDA synergy is a model of regulatory foresight. The pharmacogenomic assay leverages high‑throughput PCR and allele‑specific hybridization, delivering results within a clinically actionable window. Moreover, cost‑effectiveness analyses demonstrate that the marginal expense of $50 per test eclipses the potential $20,000–$30,000 hospitalization costs associated with hypersensitivity. This is not merely a recommendation; it is an evidentiary mandate supported by phase‑III trial data and meta‑analyses. Any clinic that neglects this protocol is essentially contravening best‑practice standards.
Esther Olabisi
October 30, 2025 AT 22:39Totally agree, the test is a game‑changer! 🌟 It’s wild how a tiny swab can keep patients from ending up in the ER. Plus, the peace of mind for clinicians is priceless. 👍
Let’s keep pushing for wider access, especially in remote areas. 😅
Rachel Valderrama
November 4, 2025 AT 13:45Sure, because waiting for a lab result is the new thrill of my day.
Brandy Eichberger
November 9, 2025 AT 04:52Dearest colleagues, your enthusiasm for precision medicine is commendable, yet one must not overlook the subtle art of patient dialogue. While the science is impeccable, it is our genteel discourse that truly convinces patients to embrace genotyping. Let us therefore pair our data‑driven recommendations with a touch of elegance.
Eli Soler Caralt
November 13, 2025 AT 19:59Ah, the eloquence of the elite! But reaaally, does it matter if we misspell a wee word when the genome itself is a chaotic poem? 🤔 Life's enigma is that even a flawed typo can spark deep thoughts… 🌌✨
Eryn Wells
November 18, 2025 AT 11:05🙌 Absolutely, let’s celebrate the diversity of our patients and ensure every community feels represented in the genomic era. Inclusion isn’t just a buzzword; it’s the foundation of equitable healthcare. 🌍💙
Angela Koulouris
November 23, 2025 AT 02:12Great points, everyone. Remember, the real win is when patients walk out confident that their treatment is both safe and personalized. Keep the momentum going, and don’t let bureaucracy stall progress.
Harry Bhullar
November 27, 2025 AT 17:19Let me unpack why this genotyping step is so pivotal. First, the HLA‑B*57:01 allele, though present in only about 5‑8% of certain populations, carries a disproportionately high risk for severe hypersensitivity reactions when patients receive abacavir. Second, the pathophysiology involves an altered peptide repertoire presented by the HLA molecule, which triggers a misguided T‑cell response-essentially a false alarm that can be life‑threatening. Third, the availability of rapid, high‑throughput PCR‑based assays means clinicians can obtain results within 24‑72 hours, fitting neatly into the initiation timeline of antiretroviral therapy. Fourth, multiple health‑economic models have demonstrated that the cost of the test is recouped many times over by preventing expensive hospital admissions and intensive care stays. Fifth, guidelines from both the FDA and CDC emphasize this testing as standard of care, reinforcing its status as a non‑negotiable step before prescribing abacavir. Sixth, the psychological benefit to patients cannot be overstated; knowing they have a green light reduces anxiety and improves adherence. Seventh, the test’s simplicity-a blood draw or buccal swab-means it can be deployed even in resource‑limited settings with proper training. Eighth, as we look toward broader pharmacogenomic panels, integrating HLA‑B*57:01 testing with other resistance and toxicity markers will streamline care further. Ninth, education of healthcare providers remains essential; many still overlook the test due to inertia or misperception of cost. Tenth, insurance coverage is improving, but advocacy is still needed to close gaps. Eleventh, community outreach can raise awareness among patients about the safety benefits. Twelfth, electronic health record alerts now automatically flag positive results, preventing accidental prescription. Thirteenth, ongoing research may reveal additional alleles influencing abacavir response, underscoring the dynamic nature of the field. Fourteenth, real‑world data from clinics that have fully implemented testing show near‑zero incidence of abacavir hypersensitivity. Finally, the overarching lesson is that precision medicine is not a futuristic luxury-it is a present‑day reality that saves lives and resources, and HLA‑B*57:01 testing is a prime example of this paradigm shift.