Acetaminophen Is Everywhere - And It’s Dangerously Easy to Overdose
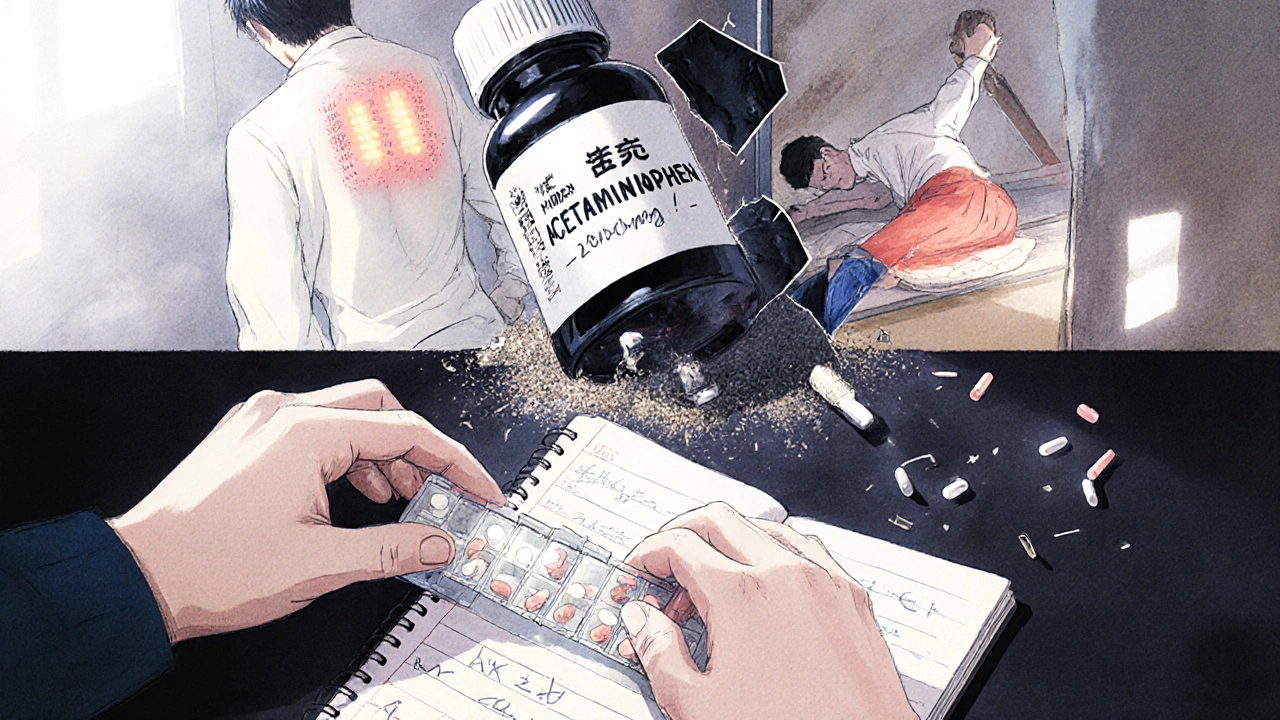
You grab a pill for your headache. Then another for your back pain. Maybe a cold medicine because you’re feeling under the weather. All seem harmless. But if you’re not careful, those pills could be quietly damaging your liver - without you even noticing until it’s too late.
Acetaminophen, the active ingredient in Tylenol and hundreds of other over-the-counter meds, is the number one cause of acute liver failure in the United States. Every year, it sends more than 56,000 people to the emergency room and kills nearly 500. And here’s the scary part: most of those cases aren’t from suicide attempts. They’re from people just trying to feel better.
Why Acetaminophen Is So Risky (Even When You Follow the Label)
Acetaminophen works fine at normal doses. Your liver breaks it down safely, mostly into harmless byproducts. But when you take too much - even just a little too much over time - your liver gets overwhelmed. It starts producing a toxic compound called NAPQI. Normally, your body neutralizes this with glutathione, an antioxidant. But when you hit around 4,000 mg in a day, glutathione runs out. That’s when NAPQI starts killing liver cells.
Here’s what most people don’t realize: 4,000 mg isn’t a lot. One regular-strength Tylenol is 325 mg. One extra-strength is 500 mg. That means eight extra-strength pills in a day hits the limit. But if you’re also taking a cold medicine that contains acetaminophen? You’ve already hit 1,000 mg before you even touch your painkiller.
And it gets worse. The FDA lowered the recommended daily limit for prescription combo pills (like Vicodin with acetaminophen) to 3,250 mg in 2021. Why? Because research showed liver damage was happening even below the old 4,000 mg threshold. So if you’re taking multiple meds, you’re playing Russian roulette with your liver.
What’s Safe If You Have Liver Disease?
If you have hepatitis, fatty liver, cirrhosis, or any other liver condition, your liver doesn’t have the same buffer. The rules change completely. The Veterans Affairs Hepatitis Resource Center says: stick to no more than 2,000 mg a day. That’s four extra-strength pills - and even that’s pushing it if you drink alcohol or take other meds.
And alcohol? Don’t even think about it. Mixing acetaminophen and alcohol - even one drink - can drop your dangerous threshold to just 2,000 mg. That’s the same as four extra-strength pills. One night out, one extra pill for a headache, and you’ve crossed the line.
NSAIDs like ibuprofen or naproxen aren’t safer alternatives. They don’t hurt the liver the same way, but they can wreck your kidneys, cause stomach bleeds, and are especially dangerous if you have advanced liver disease. Diclofenac, in particular, has been flagged as one of the most likely NSAIDs to cause liver injury. So don’t trade one risk for another.

How to Avoid Hidden Acetaminophen (The #1 Mistake People Make)
Over half of all accidental acetaminophen overdoses happen because people don’t realize they’re taking it twice. More than 600 medications contain acetaminophen - cold and flu remedies, sleep aids, prescription painkillers, even some allergy meds.
Here’s how to stop it:
- Always check the “Active Ingredients” list on every bottle - not just the brand name.
- If you see “acetaminophen,” “APAP,” or “paracetamol,” you’re taking it.
- Never combine two products that both contain it. That includes cold medicine + pain reliever.
- Use a pill organizer with daily limits marked. Write “MAX 2,000 mg” on the label if you have liver disease.
- Keep a simple log: write down every pill you take and when. Even if it’s just a note on your phone.
According to the FDA, 25% of unintentional overdoses come from people taking cold medicine on top of their regular painkiller. That’s not negligence - it’s lack of awareness. The fix? Read every label. Every time.
Signs Your Liver Is Being Damaged (Don’t Wait for Jaundice)
Acetaminophen doesn’t hurt your liver with a sharp pain. It creeps up on you. By the time you feel sick, it’s often too late. But there are early red flags:
- Nausea or vomiting (not from food)
- Loss of appetite - even your favorite foods feel gross
- Extreme fatigue that doesn’t go away
- Dark urine, like tea or cola
- Clay-colored stools
- Pain in the upper right side of your belly - right under your ribs
- Yellowing of skin or eyes (jaundice)
The National Institute of Diabetes and Digestive and Kidney Diseases says 93% of liver failure cases from acetaminophen show these symptoms within 24 to 72 hours. If you’ve taken more than the safe limit and you feel even one of these, go to the ER. Don’t wait. Don’t call your doctor tomorrow. Go now.
The antidote, N-acetylcysteine (NAC), works best if given within 8 hours of overdose. After 16 hours, it’s far less effective. Time isn’t just a factor - it’s your lifeline.
What to Use Instead of Oral Painkillers
If you need pain relief and you’re worried about your liver, there are better options:
- Topical NSAIDs: Gels or patches with diclofenac or ibuprofen go straight to the sore spot. Very little enters your bloodstream - so your liver barely sees it.
- Physical therapy: For back, knee, or joint pain, movement and strengthening help more than pills. Studies show it cuts chronic pain by 50% or more over time.
- Cognitive behavioral therapy (CBT): If your pain is long-term, CBT helps your brain rewire how it responds to pain signals. It’s not “just in your head” - it’s science.
- Acupuncture: Multiple studies, including one from the American Liver Foundation in 2024, show it reduces chronic pain without drugs.
- Heat or ice: Simple, free, and effective for muscle aches or arthritis flare-ups.
Acetaminophen is still the preferred OTC pain reliever for people with liver disease - but only if used within strict limits. The goal isn’t to avoid it completely. It’s to use it wisely.
Genetic Risk? Maybe You’re More Vulnerable Than You Think
Not everyone reacts the same way to acetaminophen. Some people naturally produce less glutathione - the liver’s natural detoxifier. That’s thanks to small genetic differences in enzymes like glutathione S-transferase.
Companies like 23andMe now offer genetic tests that can flag these variations. If you’ve had unexplained liver enzyme spikes or reacted badly to normal doses of acetaminophen, a genetic test might explain why. Even if you’re healthy, knowing you’re genetically more sensitive could mean cutting your max dose to 2,000 mg - just to be safe.
What’s Changing in 2025 (And What You Should Do Now)
The FDA now requires all OTC acetaminophen products to have a bold “Liver Warning” on the front label. That’s new since 2022. And it’s working - unintentional overdoses dropped 21% in the first year.
But here’s the real win: research is moving toward painkillers that don’t go through the liver at all. The NIH has committed $47 million to develop new analgesics that bypass liver metabolism entirely. That’s the future.
Until then, your best defense is simple:
- Know your limit: 4,000 mg max for healthy adults. 2,000 mg if you have liver disease.
- Read every label - every time.
- Never mix with alcohol.
- Use non-pill options when you can.
- Track what you take.
Your liver doesn’t complain until it’s too late. But you can protect it - if you know how.
Can I take Tylenol if I have fatty liver disease?
Yes - but only up to 2,000 mg per day, and never with alcohol. Fatty liver means your liver is already stressed, so it can’t handle extra toxins. Stick to the lowest effective dose and avoid combination meds. Always check with your doctor before starting any new pain reliever.
Is ibuprofen safer for my liver than acetaminophen?
Ibuprofen doesn’t cause direct liver damage like acetaminophen does. But it’s not safer overall. It can cause stomach bleeding, raise blood pressure, and harm your kidneys - especially if you have liver disease. For people with cirrhosis, NSAIDs like ibuprofen are often discouraged because they increase the risk of kidney failure. Topical versions are a better choice.
How do I know if a cold medicine has acetaminophen?
Look for “acetaminophen,” “APAP,” or “paracetamol” in the “Active Ingredients” section on the label. Don’t rely on the brand name. Products like NyQuil, Theraflu, DayQuil, and many store-brand cold remedies all contain it. If you’re unsure, leave it on the shelf.
What should I do if I accidentally took too much acetaminophen?
Call Poison Control immediately at 1-800-222-1222 (U.S.) or go to the nearest emergency room. Do not wait for symptoms. The antidote, N-acetylcysteine (NAC), works best within 8 hours. After 16 hours, its effectiveness drops sharply. Even if you feel fine, get checked.
Can children take acetaminophen safely?
Yes - but only with the correct dose based on weight, not age. Use the measuring tool that comes with the bottle, not a kitchen spoon. Overdoses in kids are still common because parents give multiple doses too close together or mix medicines. Always check labels and never give adult formulas to children.
Is it safe to take acetaminophen every day for chronic pain?
Taking acetaminophen daily for months or years increases your risk of liver damage, even if you stay under 4,000 mg. The liver doesn’t get a break. For chronic pain, non-drug treatments like physical therapy, acupuncture, or CBT are safer long-term. If you need daily pain relief, talk to your doctor about alternatives.
What to Do Next
Start today: Look in your medicine cabinet. Pull out every bottle - painkillers, cold meds, sleep aids. Check the active ingredients. If you see acetaminophen, APAP, or paracetamol, write it down. Add up your daily total. If you’re over 2,000 mg and have liver disease, stop. Call your doctor. If you’re healthy but take more than 3,000 mg a day, cut back. Your liver doesn’t have a voice. But you do.


Shivam Goel
November 23, 2025 AT 04:54Arup Kuri
November 24, 2025 AT 07:45Elise Lakey
November 24, 2025 AT 17:47Timothy Sadleir
November 24, 2025 AT 17:53Roscoe Howard
November 25, 2025 AT 00:17Lisa Odence
November 26, 2025 AT 09:37Agastya Shukla
November 27, 2025 AT 00:23Rachel Villegas
November 27, 2025 AT 16:15Emily Craig
November 28, 2025 AT 02:46Karen Willie
November 28, 2025 AT 07:26Leisha Haynes
November 28, 2025 AT 22:33Jefriady Dahri
November 30, 2025 AT 09:42Andrew McAfee
December 1, 2025 AT 06:37