Most women don’t realize they’re pregnant until they’re already 4 to 6 weeks along. By then, the baby’s heart, brain, spine, and all major organs have already started forming. If you’re taking certain medications during this time, you could be exposing your developing baby to risks you never knew existed. That’s why creating a medication plan before conception isn’t just a good idea-it’s essential.
Why Timing Matters More Than You Think
The first eight weeks of pregnancy are the most critical. That’s when the embryo transforms from a tiny cluster of cells into a fully formed baby with a beating heart, developing limbs, and a neural tube that becomes the brain and spinal cord. This happens before most women even miss a period. If you’re on a medication that’s harmful during this window, waiting until you’re pregnant to make changes is too late. According to the American College of Obstetricians and Gynecologists (ACOG), nearly half of all pregnancies in the U.S. are unplanned. That means a lot of women are unknowingly exposed to medications that can cause birth defects. The risk isn’t small. Some drugs can increase the chance of major congenital anomalies by 2 to 10 times. For example, valproic acid, used for epilepsy and bipolar disorder, carries a 10.7% risk of major birth defects. That’s more than 1 in 10 babies. The good news? You don’t have to accept this risk. With proper planning, you can switch to safer options, adjust dosages, or stop dangerous drugs months before trying to conceive. This isn’t about giving up treatment-it’s about protecting your future child while keeping yourself healthy.Start With a Full Medication Inventory
Don’t just think about your prescription list. Look at everything you take. That includes:- Prescription drugs
- Over-the-counter pain relievers (like ibuprofen or naproxen)
- Vitamins and supplements
- Herbal remedies and teas
- Topical creams and patches
Key Medications to Review (and What to Do Instead)
Some drugs are known teratogens-meaning they can cause birth defects. Here’s what to watch for:Antiepileptic Drugs
If you have seizures, stopping your meds isn’t an option. But some are far riskier than others. Valproic acid and topiramate should be avoided. Studies show topiramate increases the risk of cleft lip and palate by 1.4%, compared to 0.36% in the general population. Carbamazepine is safer but still carries a small risk. Your neurologist should switch you to lamotrigine or levetiracetam, which have the best safety profiles during pregnancy.Antidepressants and Mood Stabilizers
Lithium, used for bipolar disorder, can cause a rare but serious heart defect called Ebstein’s anomaly. The risk is low-about 1 in 2,000-but still significant. SSRIs like sertraline and citalopram are generally considered safer options. Never stop antidepressants cold turkey-this can trigger a relapse, which is dangerous for both you and the baby. Work with your psychiatrist to taper safely and switch if needed.Autoimmune and Arthritis Medications
Methotrexate and leflunomide are absolute no-gos. Methotrexate is a chemotherapy drug that causes severe birth defects and miscarriage. Even after stopping, it can stay in your system for months. You need at least 3 months (and preferably 6) before trying to conceive. Leflunomide requires a special washout procedure with cholestyramine. Sulfasalazine, on the other hand, is safe to continue.Diabetes and Weight Loss Drugs
If you have type 1 or type 2 diabetes, your blood sugar control before pregnancy is critical. High glucose levels in early pregnancy raise the risk of heart defects, neural tube defects, and miscarriage. Metformin is safe to use during preconception and pregnancy. But drugs like liraglutide (Victoza, Saxenda) and semaglutide (Wegovy, Ozempic) have no proven safety data in pregnancy. Stop these at least 2 months before trying to conceive.Blood Thinners
Warfarin (Coumadin) is a major red flag. It crosses the placenta and can cause fetal warfarin syndrome, which includes facial deformities, bone problems, and intellectual disability. If you’re on warfarin for a blood clotting disorder, you’ll need to switch to low-molecular-weight heparin (like enoxaparin). It doesn’t cross the placenta and is safe during pregnancy.Acne Medications
Isotretinoin (Accutane) is one of the most dangerous drugs for pregnancy. It causes severe birth defects in up to 35% of exposed pregnancies. You must stop it at least 1 month before conception and use two forms of birth control during treatment and for one month after. The iPLEDGE program requires strict compliance-don’t skip it.Folic Acid: The One Supplement Everyone Needs
Folic acid isn’t optional. It’s non-negotiable. The World Health Organization recommends 400 micrograms daily for all women of childbearing age. Why? Because neural tube defects-like spina bifida and anencephaly-can be reduced by up to 70% with proper folic acid intake before conception. But if you have certain conditions, you need more:- General population: 400-800 mcg daily
- Diabetes, obesity, epilepsy, or previous pregnancy with neural tube defect: 4-5 mg daily
Thyroid and Other Chronic Conditions
If you have hypothyroidism, your TSH level should be under 2.5 mIU/L before you get pregnant. Higher levels increase miscarriage risk by 60%. Once pregnant, your levothyroxine dose will likely need to increase by 30%-so your doctor should plan this in advance. For asthma, continue using inhaled corticosteroids. Uncontrolled asthma is far more dangerous to your baby than the medication. For high blood pressure, switch from ACE inhibitors or ARBs (like lisinopril or losartan) to methyldopa or labetalol. These are safe during pregnancy.How Long Should You Plan Ahead?
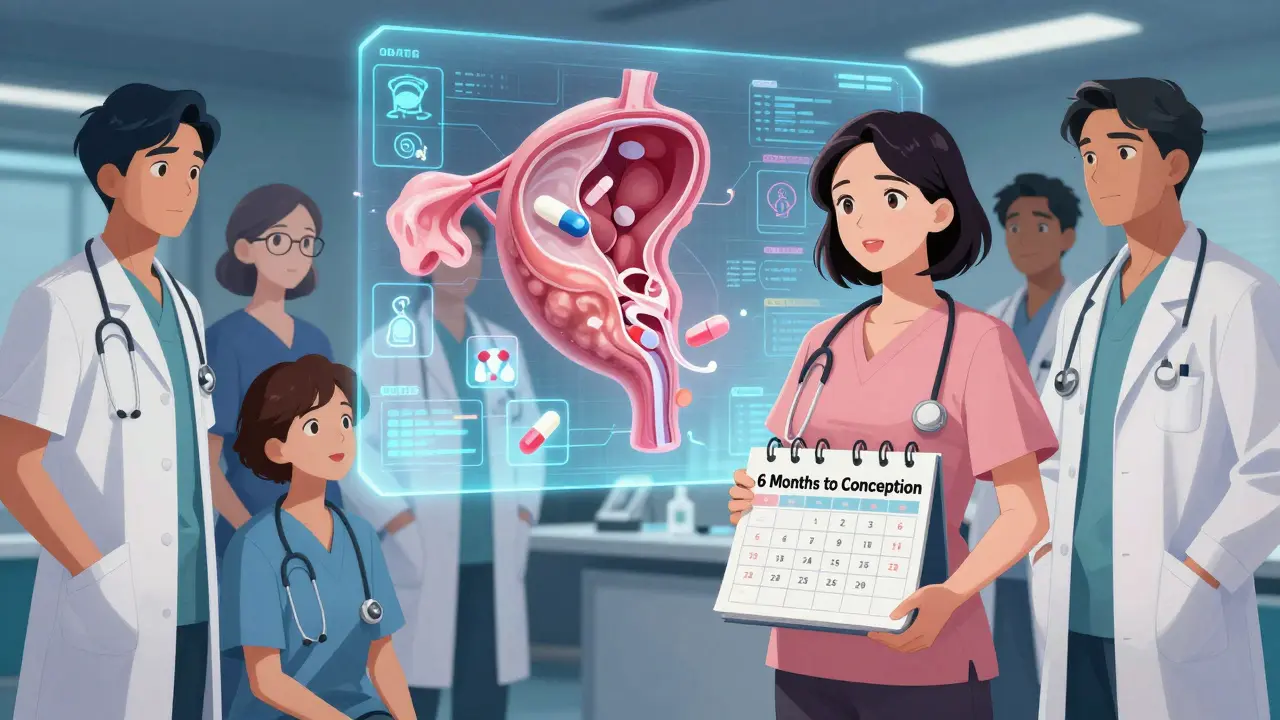
Don’t wait until you’re ready to try. Start 6 months before. Why? Because some drugs take time to clear from your system.- Methotrexate: 3 months (minimum 3 ovulatory cycles)
- Leflunomide: 2 months (with cholestyramine washout)
- Isotretinoin: 1 month
- Anticonvulsants: 2-3 months to stabilize on safer alternatives
Who Should Be on Your Team?
This isn’t a solo mission. You need a team:- Your OB/GYN or midwife
- Your primary care doctor
- Your specialist (neurologist, rheumatologist, endocrinologist, psychiatrist)
- A pharmacist who specializes in pregnancy (many hospitals have one)

What If You’re Already Pregnant?
If you’ve just found out you’re pregnant and you’re on a risky medication, don’t panic. Don’t stop anything on your own. Call your doctor immediately. Many medications are safe in early pregnancy, and some risks are lower than people think. For example, if you took ibuprofen in the first few weeks, the risk is minimal. But if you’re on valproic acid or isotretinoin, you need urgent help. Your provider can arrange genetic counseling and early ultrasounds to monitor the baby’s development.Barriers and How to Overcome Them
Only 24% of obstetric providers consistently do preconception medication reviews. Why? Time. Most appointments are 15 minutes. But that doesn’t mean you’re out of luck. - Ask for a longer appointment. Say: “I’m planning to get pregnant and need to review my medications for safety.” - Bring a printed list. Make it easy for them. - Use digital tools. Apps like Luma Health’s Preconception Navigator can help you track your meds and flag risks. - If you’re in a rural area or can’t see a specialist, your pharmacist or primary care provider can help. WHO guidelines say any trained health worker can provide basic preconception care.What’s Next?
Once your medication plan is in place, keep going:- Continue folic acid daily
- Stop alcohol, smoking, and recreational drugs
- Get your vaccines up to date (flu, whooping cough, COVID-19)
- Manage stress and sleep
- Start tracking your cycle
Can I keep taking my antidepressants if I’m trying to get pregnant?
Yes, but not all antidepressants are equal. Sertraline and citalopram are considered the safest options during pregnancy. Avoid paroxetine-it’s linked to a small increase in heart defects. Never stop your medication without talking to your psychiatrist. Untreated depression carries its own risks, including poor prenatal care and preterm birth. Work with your provider to find the lowest effective dose before conception.
Is it safe to take ibuprofen before pregnancy?
Occasional use of ibuprofen before conception is generally safe. But if you’re trying to conceive, switch to acetaminophen (Tylenol) as your go-to pain reliever. Regular use of NSAIDs like ibuprofen or naproxen may interfere with ovulation and reduce fertility. Once pregnant, avoid them entirely after 20 weeks because they can affect fetal kidney development.
Do I need to stop my birth control before trying to conceive?
You can stop hormonal birth control (pill, patch, ring) right away. Your fertility will return within weeks for most women. If you’re on an IUD or implant, have it removed. For women on enzyme-inducing epilepsy drugs (like carbamazepine), birth control pills may not work well. Use a copper IUD or condoms as backup. Don’t rely on the pill alone if you’re on these medications.
What if I’m on a medication with no known safety data?
Many newer drugs-especially weight-loss meds like semaglutide or psoriasis biologics-don’t have enough data for pregnancy. In these cases, your doctor will weigh the risk of stopping the drug (like uncontrolled disease) against the unknown risk to the baby. Often, switching to an older, better-studied alternative is the best path. Never assume a drug is safe just because it’s new.
How do I know if a medication is teratogenic?
Don’t rely on outdated pregnancy categories (A, B, C, D, X). Instead, use trusted sources like the Organization of Teratology Information Specialists (OTIS), MotherToBaby, or the FDA’s Pregnancy and Lactation Labeling Rule (PLLR) summaries. Your pharmacist or a maternal-fetal medicine specialist can also help interpret the data. If a drug has no clear safety profile, assume caution until proven otherwise.
If you’re taking any medication and thinking about pregnancy, don’t wait. Schedule a preconception visit now. Even if you’re not ready to conceive next month, this plan will give you peace of mind-and the best chance for a healthy baby.


Edith Brederode
January 21, 2026 AT 03:43Emily Leigh
January 21, 2026 AT 15:35Shane McGriff
January 21, 2026 AT 16:12Art Gar
January 23, 2026 AT 14:13Crystal August
January 25, 2026 AT 03:25Andy Thompson
January 26, 2026 AT 20:40Arlene Mathison
January 28, 2026 AT 17:10Jacob Cathro
January 29, 2026 AT 01:24Thomas Varner
January 30, 2026 AT 17:03pragya mishra
January 31, 2026 AT 11:30Manoj Kumar Billigunta
February 1, 2026 AT 02:52kumar kc
February 1, 2026 AT 13:59Renee Stringer
February 1, 2026 AT 16:29clifford hoang
February 2, 2026 AT 00:28Paul Barnes
February 3, 2026 AT 13:05