Every year, thousands of people accidentally take two doses of the same medicine-sometimes within hours-because they forgot if they already took it. It’s not laziness. It’s not carelessness. It’s confusion. And it’s happening in homes across the country, especially with older adults juggling five or more prescriptions and parents managing liquid meds for kids. The result? Emergency rooms, hospital stays, and in some cases, death. The good news? Most of these mistakes are easy to prevent with simple, proven systems.
Why Double-Dosing Happens More Than You Think
You’d think taking medicine is straightforward: pop a pill, drink water, done. But real life isn’t like that. Someone’s sick, the kids are crying, the dog barks, and you’re rushing to work. You grab your bottle, take your pill, and later-maybe after a nap, a phone call, or a walk-you think, Did I take that already? That’s when the second dose goes in. According to the National Council on Patient Information and Education, about half of all medication-related emergencies happen at home. And nearly one in four seniors admit they’ve double-dosed at least once in the past year. For kids, it’s even more dangerous: 86% of emergency visits for medicine poisoning involve children getting into meds meant for adults. The problem gets worse when multiple people are involved. A parent gives a child medicine because they’re fussy. Later, another parent gives it again because they didn’t know it was already given. Or an elderly person takes their morning pill, forgets, takes it again after lunch, and doesn’t realize until they feel dizzy.Use a Pill Organizer-But Not Just Any One
The most common and effective tool is the pill organizer. But not all of them work the same. A basic 7-day organizer with separate compartments for morning, noon, evening, and bedtime is what most experts recommend. These aren’t just for seniors. If you or someone you care for takes more than one pill a day, this is the first line of defense. Here’s how it works: Sunday morning, you fill all the slots for the week. Each day, you open the compartment and see exactly what’s left. If the slot is empty, you took it. If it’s full, you didn’t. No guessing. No anxiety. Studies show that using a pill organizer alone reduces double-dosing by 35%. But when paired with another method-like a reminder-it jumps to 62% effectiveness. That’s because the organizer doesn’t just track what you took; it shows you what you still need to take. Avoid cheap plastic organizers that don’t lock or have flimsy lids. Look for ones with clear labels and easy-to-open compartments. Some even have alarms built in. You don’t need the fanciest one-just one that’s easy to use every single day.Set Digital Reminders-And Make Them Smart
Your phone can be your best friend-or your worst enemy-when it comes to medication safety. Apps like Medisafe, MyTherapy, or even the built-in Reminders app on iOS or Android can send alerts at the exact time you need to take your meds. But here’s the trick: don’t just set one reminder for “take pill.” Set separate ones for each dose. And include the name of the medicine. For example:- 8:00 AM: Take Lisinopril 10mg
- 12:00 PM: Take Metformin 500mg
- 8:00 PM: Take Atorvastatin 20mg
Never Use Kitchen Spoons to Measure Liquid Medicine
This one catches people off guard. You’ve got a bottle of children’s acetaminophen. You don’t have the syringe. So you grab a teaspoon. Big mistake. A teaspoon from your kitchen can hold anywhere from 2.5 milliliters to 7.3 milliliters. The actual dose for a child might be 5 mL. If you use a spoon that holds 7 mL, you’ve just given 40% too much. That’s not a little extra. That’s a dangerous overdose. Always use the syringe, dropper, or cup that came with the medicine. If you lost it, go to the pharmacy and ask for a new one. They’ll give it to you for free. And never guess. If the label says “5 mL,” measure it. Don’t eyeball it. Don’t use a soup spoon. Don’t use a shot glass. Use the tool that came with the bottle.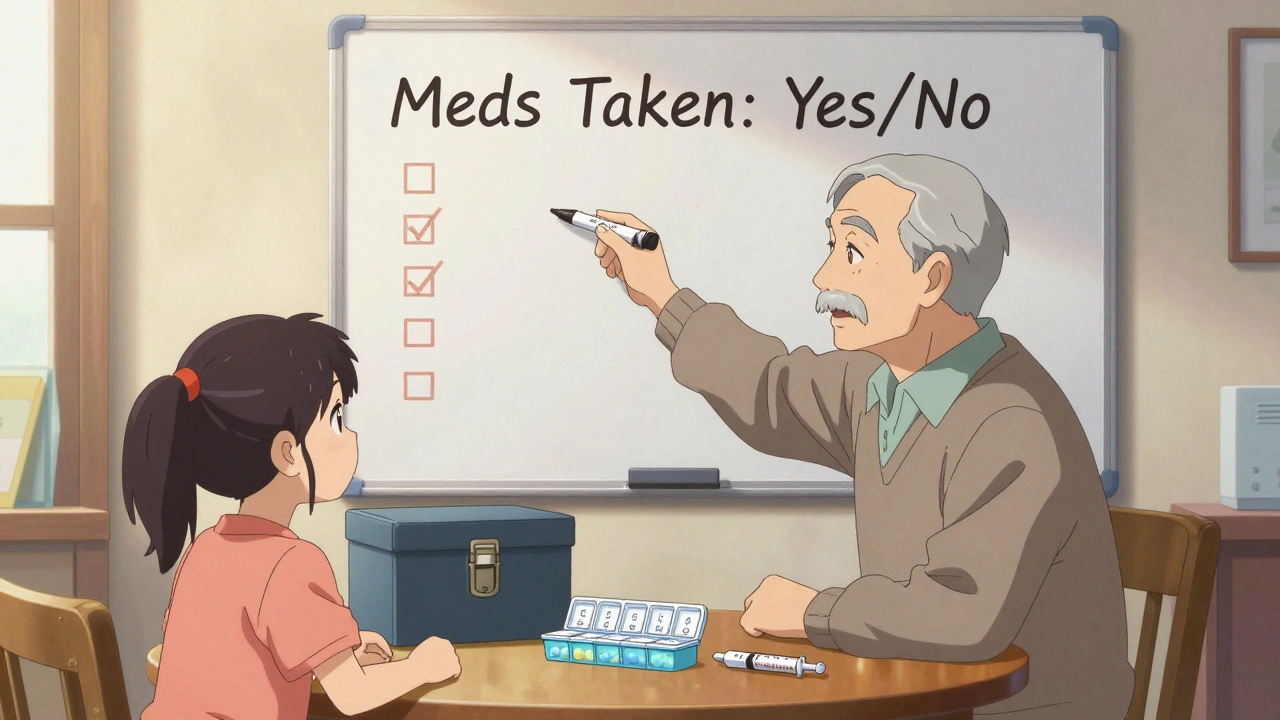
Keep a Master Medication List
You’re taking blood pressure pills, a cholesterol med, a pain reliever, a vitamin, and a sleep aid. But you also take Advil for your knee. And your wife gives you melatonin at night. And your son left his cough syrup on the counter. Now you’re double-dosing on ibuprofen without knowing it. Many over-the-counter cold and pain meds contain the same active ingredients as prescription drugs. Ibuprofen. Acetaminophen. Diphenhydramine. These are hidden in plain sight. Write down every single thing you or your loved one takes-prescription, OTC, vitamin, supplement, herbal remedy. Include the dose and time. Keep it on your phone and on the fridge. Update it every time you get a new prescription. Pharmacists at EssexCare Pharmacy say 32% of double-dosing cases they’ve seen in 2023 were caused by patients not realizing two different pills had the same ingredient. A simple list prevents that.Assign One Person to Manage the Meds
In households with multiple caregivers-parents, grandparents, nannies, adult children-it’s chaos. One person gives the medicine. Another doesn’t know. Another gives it again because the child cried and refused earlier. That’s how overdoses happen. St. Louis Children’s Hospital found that assigning one person as the “medication manager” cuts double-dosing by nearly 50% in families. That doesn’t mean that person does all the work. It means they’re the only one who gives the medicine-or at least the only one who confirms it’s been given. Use a whiteboard or a shared note on your phone. Write: “Medicine given: 8 AM.” That way, everyone sees it. No assumptions. No guesses. For older adults living alone, ask a neighbor, friend, or home care worker to check in daily. A quick call: “Did you take your pills today?” can save a life.Store Medicines Out of Reach-And Out of Sight
You can have the best system in the world, but if the medicine is on the counter, in the bathroom cabinet, or on the nightstand, someone will find it. Children’s Healthcare of Atlanta reports that most poisonings happen because kids grab meds meant for adults. That’s not because parents are negligent. It’s because medicine is everywhere. Keep all meds-prescription and OTC-in one locked box, high up, away from kids and pets. Even vitamins and supplements. Many contain iron or other ingredients that can be toxic in large doses. And never leave a pill bottle out after you’ve taken your dose. Put it back immediately. That tiny habit prevents 90% of accidental access.
Link Meds to Daily Routines
Memory is unreliable. But habits? They stick. The best way to remember your pills is to tie them to something you do every day without thinking: brushing your teeth, eating breakfast, turning off the alarm, or getting into bed. A 2023 study found that 78% of people who successfully stuck to their medication schedule linked it to a daily habit. So:- Take your morning pill right after you brush your teeth.
- Take your evening pill right before you turn off the TV.
- Take your bedtime pill right after you wash your face.
What to Do If You Accidentally Double-Dose
If you realize you’ve taken two doses, don’t panic. But don’t wait either. Call the Poison Control Center at 1-800-222-1222. They’re available 24/7. Tell them:- What medicine you took
- How much you took
- When you took it
- How old you are or how much the person weighs
Smart Tech Is Coming-But Don’t Wait for It
New devices are popping up: pill dispensers that lock after each dose, apps that alert family members if a dose is missed, smart bottles that track when they’re opened. A 2023 Johns Hopkins study found that smart dispensers reduced double-dosing by 76%. But they cost hundreds of dollars. And they’re not covered by insurance. You don’t need to wait for the future. The tools you already have-pill organizers, phone reminders, medication lists, and clear communication-are enough. They’ve been proven for years. They’re cheap. They’re simple. The key isn’t technology. It’s consistency.Final Checklist: Your Daily Medication Safety Routine
- Use a 7-day pill organizer with AM/PM slots
- Set phone reminders with medicine names
- Use the correct measuring tool for liquids
- Keep a master list of all meds and supplements
- Assign one person to give or confirm doses
- Store all meds in a locked, out-of-reach location
- Link doses to a daily habit like brushing teeth
- Call 1-800-222-1222 if you think you’ve double-dosed
What’s the most common cause of accidental double-dosing?
The most common cause is forgetting whether a dose was already taken-especially when multiple caregivers are involved, routines are disrupted, or medications are taken at irregular times. Studies show that 63% of seniors experience "Did I take my pill?" anxiety at least once a week, and nearly a third admit to double-dosing in the past year.
Can I use a kitchen spoon if I don’t have the measuring cup?
No. Kitchen spoons vary in size by up to 65%, which means you could give 2 to 3 times the intended dose. Always use the syringe, dropper, or dosing cup that came with the medicine. Pharmacies give these out for free if you lost yours.
Are pill organizers only for older adults?
No. Anyone taking more than one medication a day-whether they’re 8 or 80-can benefit. Teens on ADHD meds, parents managing asthma inhalers, or people on blood thinners all use pill organizers to stay safe and on schedule.
What should I do if I accidentally give my child two doses?
Call Poison Control immediately at 1-800-222-1222. Do not wait for symptoms. Have the medicine bottle ready to tell them the name, dose, and time given. Most cases can be managed at home with guidance, but some require urgent care.
Why do some medicines have the same ingredient in different products?
Many over-the-counter cold, flu, pain, and sleep meds contain the same active ingredients as prescription drugs-like acetaminophen, ibuprofen, or diphenhydramine. Taking both can lead to dangerous overdose. Always check the "Active Ingredients" section on the label and keep a full list of everything you take.
How can I help an elderly relative who forgets to take their meds?
Start with a weekly pill organizer and set up a daily phone reminder. Then, assign one person to check in each day. Many families use a simple whiteboard: "Meds taken: Yes/No." If they live alone, consider a home care worker or neighbor who can stop by. Even a 5-minute check can prevent a hospital visit.
Is it safe to use a pill organizer for all types of medications?
Most pills are fine, but some shouldn’t be removed from their original packaging. Medications that are sensitive to light, moisture, or air-like nitroglycerin or certain antibiotics-should stay in their original bottles. Always check with your pharmacist before transferring any meds to a pill organizer.
How often should I update my medication list?
Update it every time you get a new prescription, stop a medication, or start a new supplement. Keep a printed copy in your wallet and a digital copy on your phone. Share it with your doctor and pharmacist at every visit.


Lola Bchoudi
December 7, 2025 AT 13:44Let’s be real-most people skip the pill organizer because it’s ‘too much work.’ But here’s the thing: if you’re juggling five meds, you’re not being lazy, you’re being under-supported. A properly labeled, lockable 7-day organizer isn’t a gadget-it’s a cognitive offload. Pair it with a phone alert that says ‘Lisinopril 10mg’ and you’ve just cut your risk of ER visits by 60%. No magic. Just systems. And if you’re caring for someone elderly? Do it with them. Not for them. They need to own the routine, not just follow it.
Michael Robinson
December 7, 2025 AT 16:10It’s not about remembering. It’s about not needing to. The body doesn’t care if you forgot. It just reacts. So why make the brain do the work? Build the environment so the right thing is the only thing possible. Locked box. Same time. Same spot. No choices. No doubt. That’s not discipline. That’s design.
Andrea Petrov
December 8, 2025 AT 01:17Have you ever wondered why these ‘simple solutions’ are pushed so hard? Who benefits? Pharmacies sell organizers. App companies track your data. The FDA? They love when you self-report errors instead of suing them. And don’t get me started on ‘master lists’-they’re just Trojan horses for insurance companies to audit your prescriptions. I’ve seen it. They flag ‘unusual combinations’ and then deny coverage. This isn’t safety. It’s surveillance dressed as care.
Suzanne Johnston
December 8, 2025 AT 08:21I’ve worked in community health for 18 years, and the single most effective thing I’ve seen isn’t tech or tools-it’s connection. A neighbor checking in. A daughter calling after dinner. A quiet ‘did you take your blood pressure pill today?’ That human moment? It’s more powerful than any app. Systems help, yes. But loneliness kills faster than missed doses. If you’re managing meds for someone, don’t just fix the pillbox-fix the silence around it.
George Taylor
December 9, 2025 AT 06:02iswarya bala
December 9, 2025 AT 22:23Asset Finance Komrade
December 10, 2025 AT 13:38One must question the epistemological foundations of this ‘solutionist’ paradigm. We are being sold the illusion of control through material objects-a pill organizer, a phone app-as if cognition can be outsourced to silicone and plastic. The real issue is not memory, but alienation: we have been severed from the ritual of care. The act of taking medicine should be sacred, not mechanized. Let us return to the quiet, unmediated moment-the hand, the water, the silence. Not the alarm. Not the checklist. Not the app.
Jennifer Blandford
December 11, 2025 AT 16:54Y’all. I just used a kitchen spoon once. Just once. For my kid’s fever med. And I swear to god, I felt like a monster when I read this. 😭 I went straight to the pharmacy and got a new syringe. They gave me one for free AND a sticker that says ‘I’m a responsible parent.’ I cried. I’m not crying because I’m emotional-I’m crying because someone finally saw me. And told me it’s okay to mess up… as long as you fix it. Thank you. This post saved my soul.
Stacy Tolbert
December 13, 2025 AT 10:00I read this and immediately thought of my dad. He’s 79, takes 7 meds, and lives alone. He swears he doesn’t forget. But last week, he took his blood thinner twice and ended up in the ER with a bruise the size of a grapefruit. I didn’t know what to do. So I flew out. Bought him a locked organizer. Set up the reminders. Made a whiteboard. And now I call every day at 8 a.m. Just to say hi. And ask if he took his pills. He hates it. But he doesn’t hang up. And that’s enough.