Every time you pick up a prescription, there’s a hidden guide tucked inside the bottle - one that could literally save your life. But most people never read it. Or worse, they read it and don’t understand what they’re seeing. The safety and warnings section on your prescription label isn’t just fine print. It’s your personal alert system for dangerous side effects, deadly interactions, and life-threatening risks. If you’ve ever taken a pill and wondered, "What if this does something bad?" - this is your answer.
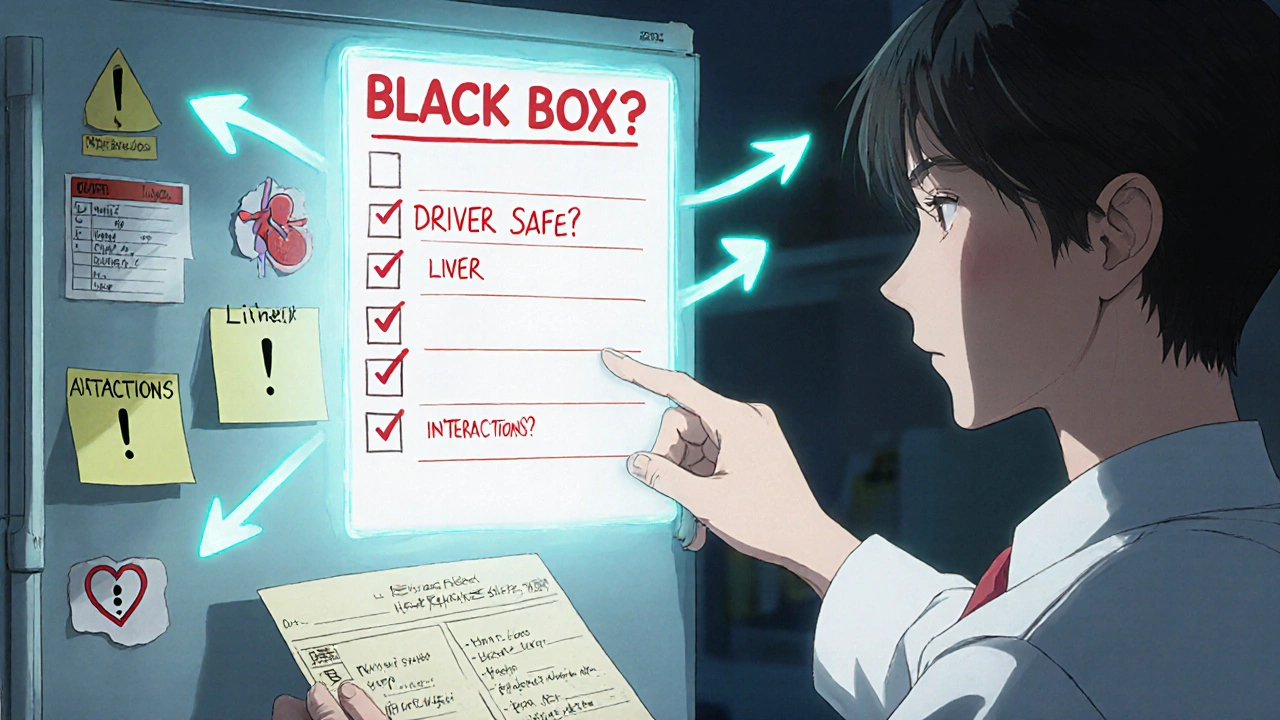
What’s in the Boxed Warning? (It’s Not Just a Box)
Look for a black rectangle on the label. That’s the boxed warning, also called a "black box warning." It’s the strongest warning the FDA can require. If your medication has one, it means serious harm - even death - has happened to people who took it. This isn’t a suggestion. It’s a red flag. For example, clozapine, used for severe schizophrenia, carries a boxed warning for agranulocytosis - a condition where your body stops making white blood cells. Without regular blood tests, this can kill you. Another example is fluoroquinolone antibiotics like ciprofloxacin. Their boxed warning says they can cause permanent nerve damage or tendon rupture. If you’re on one of these, you need to know why you’re taking it and what signs to watch for. The FDA requires these warnings to be printed in bold, black-bordered text, usually 8-10 point font. But here’s the problem: if the label is small - like for pediatric meds - the box might be shrunk down, or the text cut short. That’s why you can’t just glance at it. You need to read every word.Warnings and Precautions: What the Doctor Didn’t Tell You
Right after the boxed warning comes the "Warnings and Precautions" section. This is where the real details live. It’s not just "side effects" - it’s about risks you might not expect. For example:- "May cause drowsiness" - that’s not just annoying. It means don’t drive or operate machinery.
- "Has been associated with liver injury" - that means get your liver checked every few months.
- "Use with caution in patients with kidney disease" - if you have kidney problems, your dose might need to be lowered.
Drug Interactions: The Silent Killer
You take your blood pressure pill. Your neighbor says, "Try this herbal tea for stress." That tea might be St. John’s Wort - and it can make your blood pressure med useless. Or worse, cause your heart to race dangerously. The drug label’s "Drug Interactions" section doesn’t just say "avoid alcohol." It tells you exactly how the drugs clash. For example: "CYP3A4 inhibitors may increase plasma concentrations of this drug by up to 400%." That’s science-speak for: "If you take this with grapefruit juice, or certain antibiotics, your body will absorb way too much - and you could overdose." Most people don’t know what CYP3A4 means. And you don’t need to. What you do need to know is: anytime you start a new medicine, supplement, or even a big change in diet, check the interaction list. A 2022 report from the Institute for Safe Medication Practices found that 41% of medication errors happened because patients didn’t realize their 5+ daily pills could react with each other.
Pharmacy Labels: The Small Print That Matters
The big label inside the box? That’s the full prescribing info. But the one stuck on your bottle? That’s what you’ll actually see. And it’s often the most important. Pharmacies are required to print critical warnings in at least 10-point font - and in plain language. Look for stickers like:- "May cause drowsiness - do not drive or operate machinery."
- "Take on an empty stomach - wait 2 hours after eating."
- "Do not take with SSRIs - risk of serotonin syndrome."
Why You Can’t Trust Your Memory
You took this pill last month. You remember the side effects. Or do you? A 2012 study from Northwestern University found that patients with low health literacy were 3.2 times more likely to misunderstand warnings - especially ones with numbers. "Take 2 tablets twice daily" becomes "Take 4 tablets once a day." "Maximum 4 doses in 24 hours" becomes "I can take one every 6 hours - that’s 4, right?" Your brain fills in the gaps. That’s why the "teach-back" method works. Ask your pharmacist: "Can you explain why this warning matters for me?" Then repeat it back. If you can’t explain it simply, you don’t understand it yet. A 2018 study showed that when pharmacists used this method with Medicare patients, medication errors dropped by 27%. That’s not a small number. That’s lives saved.What to Do When You’re on 5+ Medications
If you’re juggling multiple prescriptions, you’re at higher risk. One pill might be fine alone. But with three others? That’s a minefield. Create a simple "warning log." Write down:- The drug name
- The warning (copy it exactly)
- What you need to avoid (food, other meds, activities)
- What symptoms to watch for
Digital Tools: QR Codes, Apps, and NFC Tags
Newer prescriptions sometimes have QR codes or NFC chips on the bottle. Scan it with your phone - and you’ll get a short video explaining the warning in plain language. Walgreens piloted this in 2022. Patients who used it understood the warnings 92% of the time. Traditional labels? Only 63%. Apps like Medisafe scan your pills and warn you about interactions. They’re not perfect, but they catch 89% of risks when used consistently. Still, these tools won’t help if you don’t have a smartphone or internet access. That’s why analog solutions - like printed warning logs and clear pharmacy stickers - still matter. The FDA is pushing for both digital and paper options to coexist.What You Should Ask Your Pharmacist
You don’t need to be a doctor to understand your label. But you do need to ask the right questions:- "Is there a boxed warning on this? What does it mean for me?"
- "What’s the most serious side effect I should watch for?"
- "What other medicines, supplements, or foods should I avoid?"
- "What symptoms mean I need to call my doctor right away?"
- "Can you show me the warning on the bottle? I want to make sure I didn’t miss anything."
Final Check: The 5-Second Rule
Before you take any new prescription, do this:- Look for the black box. Read it.
- Check the pharmacy sticker. Read it.
- Ask: "What’s the one thing I absolutely must not do?"
- Write it down.
- Ask your pharmacist to confirm your understanding.
Medication errors from misunderstood warnings cost the U.S. healthcare system over $42 billion a year. But for you? It’s not about money. It’s about safety. Your body. Your health. Your life.
What does a boxed warning mean on a prescription label?
A boxed warning, also called a black box warning, is the strongest safety alert the FDA requires. It means the drug has been linked to serious or life-threatening risks - like organ failure, severe allergic reactions, or death. These warnings are printed in a black border and must be clearly visible. If your medication has one, you need to know exactly what it means and what signs to watch for.
Why do some drug labels say "may cause" and others say "has been associated with"?
The wording tells you how strong the evidence is. "May cause" means the side effect has been reported in clinical trials or patient use - it’s possible. "Has been associated with" means it’s been observed in studies, but not always directly caused by the drug. Both mean you should pay attention. Neither is a guarantee - but both are red flags.
Can I ignore a warning if I’ve taken the drug before without problems?
No. Your body changes. So do your other medications, your diet, your age, and your health conditions. A warning that didn’t affect you last year might be dangerous now. For example, a drug that was safe with one kidney function level might become risky if your kidneys decline. Always read the label every time - even if you’ve taken it before.
What should I do if I don’t understand a warning on my label?
Don’t guess. Don’t search online and trust random websites. Call your pharmacist or doctor and ask them to explain it in simple terms. Say: "Can you tell me what this means for me?" Then repeat it back to them. If you can’t explain it simply, you don’t understand it yet. That’s how you stay safe.
Are digital warnings (QR codes, apps) better than printed ones?
They’re more effective - but not for everyone. Studies show patients who scan QR codes or use apps like Medisafe understand warnings 92% of the time, compared to 63% with printed labels. But if you don’t have a smartphone, internet access, or digital skills, printed warnings are still essential. The best approach is to use both: scan if you can, but always read the physical label too.
What if the warning on my bottle is too small to read?
By law, pharmacy-applied warnings must be at least 10-point font and clearly visible. If it’s too small, ask your pharmacist to print a larger version or provide a written copy. In some states, like California, they’re required to provide translations and larger print upon request. Never take a medication if you can’t read the warning - it’s not worth the risk.
Can I skip a warning if I’m only taking the drug for a few days?
No. Even short-term use can trigger serious reactions. For example, a single dose of certain antibiotics can cause tendon rupture. A few days of a painkiller can trigger liver damage in someone with undiagnosed liver issues. Duration doesn’t eliminate risk. Always follow every warning, no matter how short the course.

Mamadou Seck
October 31, 2025 AT 19:41Anthony Griek
November 2, 2025 AT 09:50Norman Rexford
November 2, 2025 AT 21:26Wayne Keller
November 4, 2025 AT 15:27Shana Labed
November 4, 2025 AT 19:49California Daughter
November 5, 2025 AT 21:57Vishwajeet Gade
November 6, 2025 AT 11:03Casey Crowell
November 7, 2025 AT 21:33