What Is Meibomian Gland Dysfunction?
Meibomian gland dysfunction, or MGD, is the most common cause of dry eyes you’ve never heard of. It’s not just about your eyes feeling dry-it’s about the tiny oil glands in your eyelids that have stopped working right. These glands, called meibomian glands, sit along the edge of your eyelids and secrete a clear oil that forms the outer layer of your tear film. Without this oil, your tears evaporate too fast, leaving your eyes burning, gritty, and red.
MGD isn’t one simple problem. It comes in two main forms: obstructive MGD, where the glands get clogged like a blocked drain, and hypersecretory MGD, where they produce too much oil-but it’s thick, gunky, and useless. About 86% of people diagnosed with dry eye disease actually have MGD as the root cause, according to the American Academy of Ophthalmology. That means if you’ve been told you have dry eyes and nothing seems to help, MGD might be the real issue.
Why MGD Gets Worse Over Time
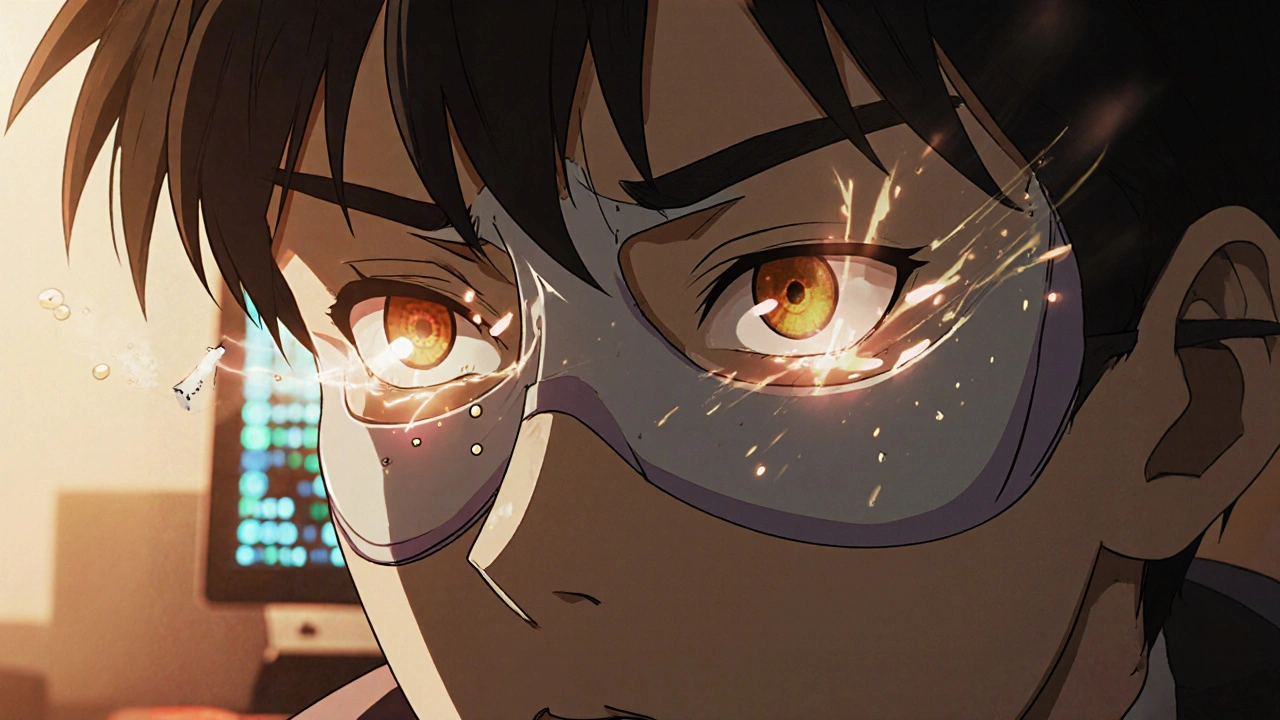
Left untreated, MGD doesn’t just stay annoying-it gets worse. The glands start to shrink, then disappear. This is called gland atrophy, and once it happens, the damage is often permanent. Studies show that patients who wait more than five years before getting help have 37% worse outcomes than those treated within the first year. The longer you wait, the more likely you are to need invasive treatments-or worse, never fully recover.
Why does this happen? Daily habits play a big role. Staring at screens for hours reduces blinking by up to 60%, which means the oil doesn’t get pushed out of the glands. Wearing eye makeup, especially waterproof mascara or eyeliner applied too close to the lash line, can clog the gland openings. Even sleeping with your face pressed into a pillow can squeeze and distort the glands over time.
Home Care: The Foundation of MGD Treatment
No matter what in-office treatment you get, nothing works without daily home care. Think of it like brushing your teeth-you wouldn’t expect a cleaning at the dentist to fix years of neglect if you never brush again. For MGD, the daily routine is simple but non-negotiable.
- Apply a warm compress for 5-10 minutes. Use a Bruder mask heated to 40-42°C, or a clean washcloth soaked in warm (not hot) water. The heat melts the hardened oil in the glands.
- Follow with gentle lid massage. Use your clean fingertip to press along the upper and lower eyelids, moving from the outer corner toward the nose. This pushes the melted oil out.
- Clean the eyelid margins with a hypochlorous acid solution or lid scrub. Products like OCuSOFT Lid Scrub remove bacteria and debris that worsen inflammation.
Studies show you need at least 85% compliance with this routine to keep symptoms under control. That means doing it every day, even when your eyes feel fine. Skip a few days, and symptoms creep back in-often within a week.
In-Office Treatments: What Actually Works
If home care isn’t enough, your eye doctor may recommend one or more in-office procedures. Not all are created equal.
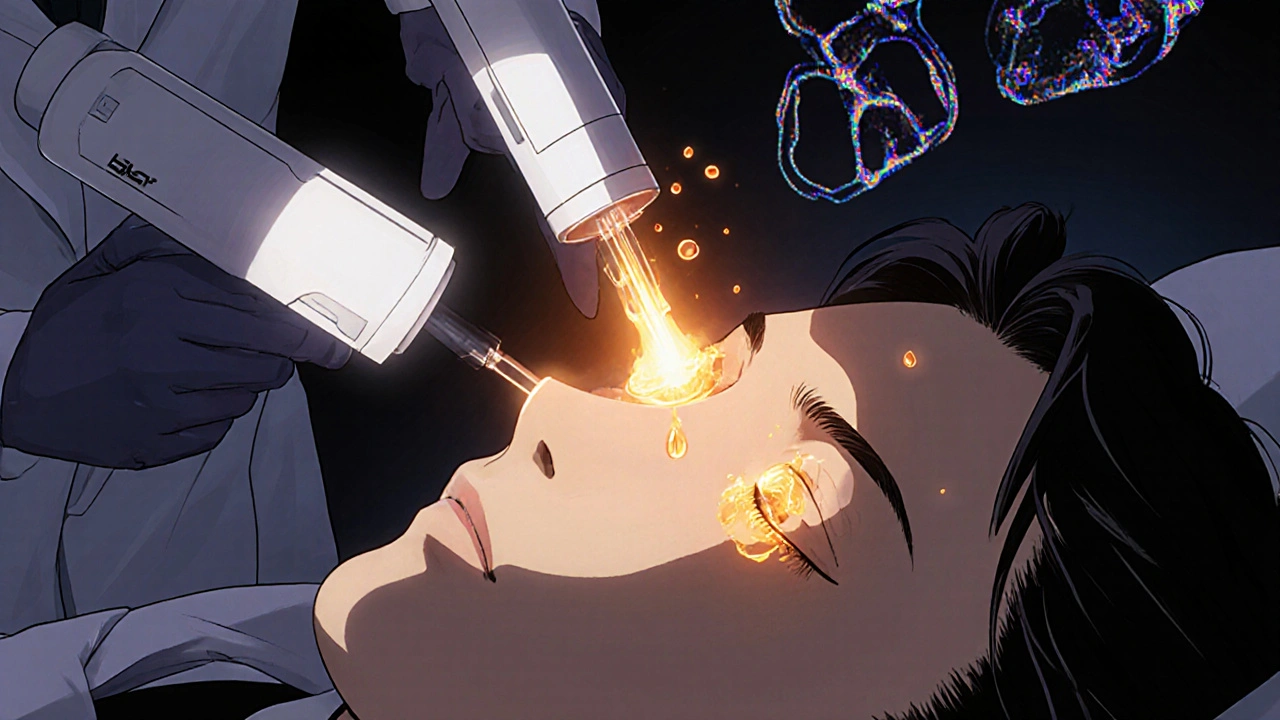
LipiFlow is the most studied thermal pulsation system. It uses heat and gentle pressure to melt and express blocked oil from the glands. A single session takes about 12 minutes per eye, and clinical trials show 68% of patients with obstructive MGD see lasting improvement in oil quality. But it costs $1,500-$2,500 per eye, and most insurance plans won’t cover it.
IPL (Intense Pulsed Light) isn’t a laser-it’s a flash of broad-spectrum light that targets redness and inflammation around the eyelids. It’s often paired with manual gland expression. Studies show IPL with expression drops OSDI scores (a measure of dry eye severity) from 32.6 to 18.3 in just four sessions. But IPL alone doesn’t clear blockages. It must be combined with expression to work.
Meibomian Gland Probing (MGP) is a more aggressive option. A thin probe is inserted into each gland to physically break up blockages deep inside the ducts. It’s usually done under local anesthetic and is most effective for advanced cases with fibrosis. Dr. Scheffer Tseng says this is the only treatment that addresses the root cause of chronic obstruction-periductal scarring. But it’s not widely available and can be uncomfortable.
Medications: When Pills and Drops Help
Some patients need help reducing inflammation or fighting infection.
Oral azithromycin is now the preferred antibiotic over doxycycline. A five-day course (500 mg on day one, then 250 mg daily) cuts inflammation and improves oil quality. One study showed 78.6% of patients had less redness after azithromycin, compared to 62.3% with doxycycline. Side effects? Only 3.2% had nausea or diarrhea-versus 28.6% with doxycycline.
Topical lifitegrast is an anti-inflammatory eye drop approved for moderate to severe dry eye. In stage 4 MGD (the most advanced), it reduced corneal staining scores by more than 50% in 12 weeks. It’s expensive and needs to be used twice daily, but it’s one of the few treatments proven to heal surface damage.
Don’t rely on over-the-counter artificial tears alone. They only mask symptoms. Without fixing the oil layer, your tears will keep evaporating.
What Doesn’t Work (And Why)
There’s a lot of noise out there. Some treatments sound great but lack proof.
The U.S. Department of Veterans Affairs classifies thermal evacuation therapies like LipiFlow as “investigational” because long-term data is still limited. That doesn’t mean they don’t work-it means insurance companies won’t pay for them. The same goes for many newer devices: they’re FDA-cleared, but not always covered.
Also, don’t assume one treatment is enough. Patients who use only one method-say, just warm compresses or just IPL-have only a 48% success rate at 12 months. Those who combine home care with one in-office procedure have a 79% success rate.
And if you have more than 50% gland dropout on meibography (an imaging test), don’t expect miracles. Structural damage can’t be reversed. Your goal shifts from restoration to management.
Real Patient Experiences
On Reddit, a user named DryEyeWarrior87 wrote: “After three LipiFlow sessions over 18 months, my OSDI score dropped from 48 to 18. But if I skip my warm compresses for a week, I’m back to square one.”
Another user, MGDstruggles, had stage 4 MGD: “LipiFlow gave me two months of relief. IPL with expression worked better, but it cost $2,000 per session. Insurance denied every claim.”
These stories aren’t rare. In a survey of 3,215 patients, 82% were happy with combined MGP and LipiFlow-but only 43% kept up with daily care after six months. And that’s the biggest reason treatments fail: consistency.
What’s Coming Next
The field is evolving fast. Exosome therapy-using tiny biological messengers to repair damaged glands-is showing 92% improvement in early trials. New nanomicellar eye drops like Cequa are penetrating deeper into the eye, delivering cyclosporine more effectively. And researchers are now looking at genetic markers, like IL-17 pathway involvement, that could lead to targeted biologic treatments.
The 2023 Dry Eye Workshop II now recommends treating MGD even before cataract surgery-even if you don’t have symptoms. Why? Because untreated MGD increases post-surgery inflammation by 40%.
How to Get Started
- See an eye doctor who specializes in dry eye or cornea. General ophthalmologists miss MGD in 65% of cases.
- Ask for meibography-an imaging test that shows the structure of your glands.
- Start daily warm compresses and lid hygiene today. No waiting.
- If symptoms persist after 6-8 weeks, ask about IPL or LipiFlow.
- Ask about azithromycin if you have redness or crusting.
- Don’t give up. MGD is chronic, but it’s manageable.
Final Thoughts
MGD isn’t a quick fix. It’s a lifelong condition that requires daily attention. But with the right combination of home care, targeted treatments, and early intervention, you can stop the decline-and even reverse some of the damage. The key isn’t finding the most expensive device. It’s sticking with the basics, knowing when to escalate, and avoiding the trap of thinking one treatment will solve everything.
Start today. Your eyes will thank you in six months.

Reema Al-Zaheri
November 20, 2025 AT 12:11Finally, a clear, evidence-based breakdown of MGD-thank you. I’ve been told ‘just use artificial tears’ for years, but the real issue was gland atrophy. I started warm compresses and lid scrubs six months ago; my OSDI score dropped from 41 to 19. Consistency is everything. Skipping even two days brings back the grittiness.
Joe Durham
November 20, 2025 AT 14:41This is one of the most thoughtful, well-researched posts I’ve seen on dry eye. I’ve struggled with this for over a decade, and I wish I’d known about meibography sooner. The part about gland dropout being irreversible hit hard-but it also gave me clarity. I’m not failing; my body just needs a different kind of care now.
Derron Vanderpoel
November 22, 2025 AT 02:04okay so i just got lipiflow last week and my eyes felt like i’d been punched in the face for three days?? like, i thought it was supposed to feel like a warm hug?? but now?? i can actually see my eyelashes again?? and i haven’t had to blink 10x to clear my vision?? i’m not crying (i swear) but this is the first time in 7 years i didn’t reach for drops before coffee
Timothy Reed
November 23, 2025 AT 01:57Thank you for this comprehensive overview. The distinction between obstructive and hypersecretory MGD is often overlooked, and the emphasis on daily hygiene as foundational-not optional-is critical. Many patients seek a ‘magic bullet,’ but sustainable improvement requires behavioral adherence. The data on compliance and outcomes is compelling: 85% adherence yields 79% success. This is not a treatment; it’s a lifestyle adjustment, akin to managing hypertension or diabetes.
Steve and Charlie Maidment
November 23, 2025 AT 20:12Look, I get that this is all very science-y and you probably think you're helping, but have you ever considered that maybe the whole dry eye thing is just a big pharma scam? I mean, why do you think they invented 17 different expensive machines? Why not just tell people to stop looking at screens? Or maybe it's all just stress? I went to a chiropractor and he said my tear ducts were 'misaligned' from sitting wrong at my desk. He gave me a $200 pillow. My eyes feel fine now. Maybe we're all just supposed to sleep more and stop trusting doctors?
Andrew Montandon
November 25, 2025 AT 16:14Important point about azithromycin over doxycycline-this is huge. I was on doxycycline for three months and felt like a zombie. Then my doctor switched me to azithromycin-five days, no nausea, and my redness vanished in a week. Also, if you’re using eyeliner? Don’t. Not even ‘waterproof.’ I used to think it was fine as long as I washed it off-but no. The oil glands are so delicate. I switched to just brow gel and my life changed. Seriously. Try it.
Sam Reicks
November 26, 2025 AT 15:57lipiflow is a scam the government and big eye companies made up to get you to spend money so they can buy more yachts. The real cause of MGD is 5g radiation from your phone. They don't want you to know that. I put my phone in the freezer at night and my glands started working again. Also, blink backwards. It's in an ancient egyptian text. I saw it on a forum. Trust me
Chuck Coffer
November 27, 2025 AT 11:21So you spent $2,000 on IPL… and still didn’t fix your life? How many years did you wait before you finally decided to care? You’re not a victim-you’re a procrastinator with a credit card. And now you’re mad because the world doesn’t owe you perfect eyelids? Maybe if you didn’t sleep face-down on your pillow like a sloth, you wouldn’t need all this.
Marjorie Antoniou
November 27, 2025 AT 13:51Thank you for sharing this. I’ve been reading about MGD for months and this is the first time I felt understood. I was embarrassed to admit I couldn’t wear mascara anymore. But now I know it’s not vanity-it’s physiology. I’m starting the warm compresses tomorrow. No more guilt. Just action.
Frank Dahlmeyer
November 27, 2025 AT 19:01I’ve been doing this for two years now-daily compresses, lid scrubs, azithromycin every six months-and I still have flare-ups. But here’s the thing: I used to think I was broken. Now I think I’m managing a chronic condition, like someone with asthma. I don’t blame myself when I sneeze-I don’t blame myself when my eyes burn. I just do the next thing. The science is solid. The key isn’t perfection-it’s persistence. You don’t need to be perfect. You just need to show up. Every. Single. Day.
Codie Wagers
November 29, 2025 AT 10:12What if MGD isn’t a disease at all? What if it’s a signal? A metaphysical protest from your body against the digital age? You’re not supposed to stare at screens for 12 hours a day. You’re not supposed to wear makeup on your tear ducts. You’re not supposed to sleep on your face. The glands aren’t broken-they’re screaming. We’ve forgotten how to be human. The real treatment isn’t heat or probes-it’s silence. Look away from the light. Breathe. Let your eyes rest. Maybe then, they’ll remember how to weep properly.
Paige Lund
November 30, 2025 AT 05:08Wow. So after all this, the answer is… do the same thing you were told to do five years ago? Groundbreaking.
Michael Salmon
December 1, 2025 AT 00:19Let’s be real: 82% of people who combine MGP and LipiFlow are happy? That’s just because they’re desperate. The real success rate? 43% stick with daily care. That means 57% gave up. So what’s the point? You’re just delaying the inevitable. Your glands are dying. You’re just buying time with money and effort. And for what? To be able to wear contacts for 8 hours instead of 4? This isn’t medicine. It’s a luxury service for people who can afford to care.
harenee hanapi
December 2, 2025 AT 13:29I’ve had MGD since I was 16 and now I’m 34 and I’ve tried EVERYTHING. I’ve done IPL, LipiFlow, probing, even tried drinking coconut oil. Nothing works. I’m just waiting for my eyes to fall out. I cried today because I couldn’t open them without pain. And now you’re telling me to do warm compresses? Like I haven’t already? Like I’m not already trying? This isn’t advice. It’s a slap in the face.
Nick Lesieur
December 2, 2025 AT 20:11you said to see a cornea specialist but what if your insurance says no? what if you live in a town with 2 doctors and one of them is a jerk who says 'just use drops'? what if you're on medicare and lipiflow costs more than your car? this whole thing is a rich person's disease. i'm not mad, i'm just disappointed.