PPI Selection Tool for Clopidogrel Users
Your Clopidogrel Interaction Risk
Recommended Alternatives
When you take clopidogrel to prevent blood clots after a heart attack or stent placement, you need it to work - not just sit in your system. But if you’re also taking omeprazole for heartburn, you might be quietly reducing clopidogrel’s power. This isn’t a guess. It’s a well-documented drug interaction rooted in your liver’s chemistry, and it can change your risk of another heart event.
How Clopidogrel Actually Works (It’s Not What You Think)
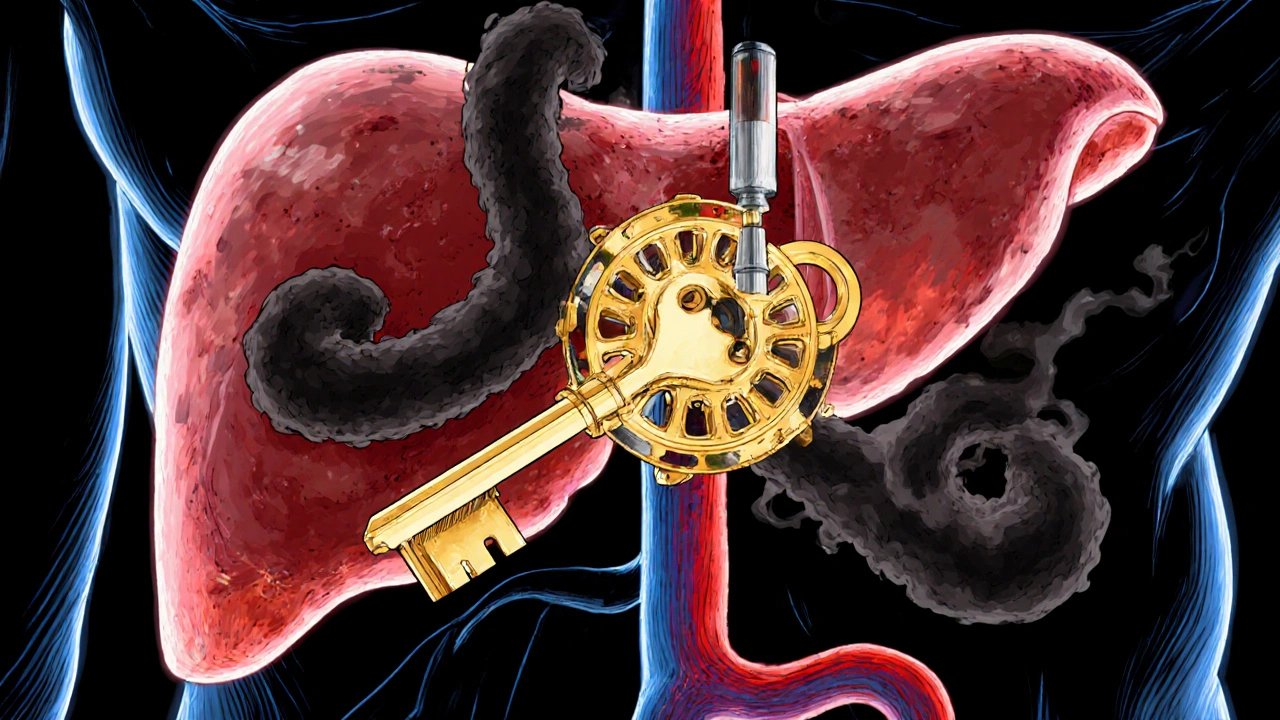
Clopidogrel doesn’t stop platelets directly. It’s a prodrug, meaning your body has to turn it into something active. That transformation happens in the liver, mostly through an enzyme called CYP2C19. Without this step, clopidogrel is useless. Think of it like a key that only works after being cut by a specific machine - CYP2C19 is that machine.
Once activated, clopidogrel binds to platelets and blocks them from clumping together. That’s how it prevents clots that cause heart attacks and strokes. But if something shuts down that liver machine - like omeprazole - the key never gets cut. And your blood stays more likely to clot.
Why Omeprazole Is the Problem (Not All PPIs)
Omeprazole, sold as Prilosec and other brands, is one of the most common proton pump inhibitors (PPIs) used for acid reflux and ulcers. But it’s also one of the strongest inhibitors of CYP2C19. Studies show that even a standard 20mg daily dose of omeprazole reduces the amount of active clopidogrel in your blood by 32%. At higher doses - like 80mg - that drop jumps to nearly 50%.
That’s not a small effect. It’s enough to interfere with how well clopidogrel protects your heart. In lab tests, omeprazole binds tightly to CYP2C19, blocking the enzyme from doing its job. Other PPIs? Not so much. Pantoprazole (Protonix) and rabeprazole (Aciphex) barely touch CYP2C19. Esomeprazole (Nexium), which is just the more active form of omeprazole, acts almost identically - so it’s just as risky. Lansoprazole (Prevacid) is in the middle. And ilaprazole, a newer PPI, shows almost no interference.
Here’s a quick comparison of how these PPIs stack up against CYP2C19:
| PPI | Typical Daily Dose | Reduction in Clopidogrel Active Metabolite | Clinical Risk Level |
|---|---|---|---|
| Omeprazole | 20-80 mg | 32-49% | High |
| Esomeprazole | 20-40 mg | 35-40% | High |
| Lansoprazole | 30 mg | Up to 18% (at 60 mg) | Moderate |
| Pantoprazole | 40 mg | ~14% | Low |
| Rabeprazole | 20 mg | ~28% (peak levels only) | Low |
| Ilaprazole | 10 mg | Negligible | Very Low |

The Real Question: Does This Actually Hurt Patients?
This is where things get messy. Yes, lab data shows omeprazole reduces clopidogrel’s active form. Yes, platelet tests show weaker antiplatelet effects. But does that translate into more heart attacks or strokes?
Some big studies say yes. A 2014 meta-analysis of over 270,000 patients found that people taking clopidogrel with any PPI had a 27% higher risk of cardiovascular events. Omeprazole alone pushed that risk up by 33%. Other studies, like the COGENT trial, found no increase in events - but that study used a low dose of omeprazole (10mg), and most patients weren’t genetically tested.
Then there’s the FAST-MI Registry, which tracked 2,744 patients and found no link between PPI use and heart events. But here’s the catch: two-thirds of those taking PPIs were on omeprazole. So if omeprazole is the main culprit, and it’s hiding in the data, the signal gets lost.
Genetics add another layer. About 30% of East Asians and 20-25% of Caucasians carry a gene variant (CYP2C19*2 or *3) that makes their liver enzyme work poorly. If you’re one of them - and you take omeprazole - your clopidogrel’s effectiveness can drop by over 50%. In one Korean study, these patients had nearly double the risk of stent clots compared to those not taking omeprazole.
What Doctors Should Do (And What You Should Ask)
Major guidelines are clear: avoid omeprazole and esomeprazole if you’re on clopidogrel. The American Heart Association, European Society of Cardiology, and FDA all warn against it. But they don’t say to avoid all PPIs.
If you need stomach protection while on clopidogrel, here’s what works:
- Use pantoprazole (40mg daily) - it’s the safest PPI option based on current data.
- Or try rabeprazole (20mg daily) - minimal interaction, though slightly less studied.
- Consider famotidine (Pepcid) - an H2 blocker that doesn’t touch CYP2C19. It’s less potent than PPIs for acid control, but safe with clopidogrel.
- Ask about switching antiplatelet drugs - prasugrel or ticagrelor don’t rely on CYP2C19. They’re stronger, faster, and unaffected by PPIs. But they carry higher bleeding risks, so they’re not for everyone.
And no, splitting your doses - taking clopidogrel in the morning and omeprazole at night - doesn’t help. The enzyme gets blocked regardless of timing. It’s not about when you take it. It’s about whether omeprazole is in your system at all.

Testing Your Genes Might Be the Best Move
More cardiology clinics are now doing CYP2C19 genetic testing. If you’ve had a stent or heart attack and need long-term clopidogrel, ask your doctor: “Should I get tested for CYP2C19 variants?”
If you’re a normal metabolizer, the risk from omeprazole is lower - but still present. If you’re an intermediate or poor metabolizer, omeprazole could be dangerously counterproductive. In those cases, guidelines strongly recommend switching to prasugrel or ticagrelor - even if you need a PPI.
As of 2023, 74% of U.S. cardiology practices are using some form of pharmacogenetic testing for patients on clopidogrel. It’s not perfect, but it’s the most precise way to avoid this interaction.
What’s Changing in 2025?
The field is moving fast. New PPIs like ilaprazole show almost no CYP2C19 inhibition, making them promising alternatives. And new antiplatelet drugs in clinical trials are being designed to bypass CYP2C19 entirely - no more liver bottlenecks.
Regulators are also updating how they assess drug interactions. The FDA now uses a more precise model called the R-value, which calculates risk based on drug concentration and enzyme binding. Omeprazole scores above the danger threshold. Pantoprazole doesn’t.
The bottom line? The interaction isn’t theoretical. It’s measurable, predictable, and avoidable. You don’t have to choose between protecting your stomach and your heart. You just need to pick the right drugs.
Can I take omeprazole with clopidogrel if I only take it once in a while?
No. Even occasional use of omeprazole can inhibit CYP2C19 long enough to reduce clopidogrel’s effectiveness. The enzyme doesn’t reset quickly, and the risk builds over time. If you need stomach protection, switch to pantoprazole or famotidine instead.
Is esomeprazole safer than omeprazole?
No. Esomeprazole is the S-isomer of omeprazole and has nearly identical effects on CYP2C19. It reduces clopidogrel’s active metabolite by about 40% - just as harmful. Avoid it just like omeprazole.
What if I’m on clopidogrel and already taking omeprazole? Should I stop?
Don’t stop either drug without talking to your doctor. But do schedule a review. Ask if you can switch to pantoprazole or famotidine. If you’ve had a stent or heart attack recently, your risk is higher. Your doctor may also consider switching you to ticagrelor or prasugrel, which aren’t affected by PPIs.
Do all PPIs interfere with clopidogrel?
No. Only omeprazole and esomeprazole strongly block CYP2C19. Pantoprazole, rabeprazole, and ilaprazole have minimal or no effect. H2 blockers like famotidine don’t interfere at all. You don’t need to avoid all acid reducers - just the ones that hit CYP2C19 hard.
Why do some studies say there’s no risk?
Some studies didn’t account for genetics or used low omeprazole doses. Others grouped all PPIs together, hiding omeprazole’s strong effect. The COGENT trial used 10mg omeprazole - below the dose where risk becomes clear. Real-world data from large registries often show mixed results because they include patients who aren’t genetically vulnerable. But for high-risk patients, the evidence is clear: avoid omeprazole.

George Clark-Roden
November 3, 2025 AT 08:52It’s wild how something as simple as heartburn medicine can quietly sabotage a life-saving drug-like swapping your car’s fuel with water and wondering why the engine sputters. CYP2C19 isn’t just some enzyme you can ignore; it’s the locksmith that cuts the key to clopidogrel’s power. And omeprazole? It’s not just interfering-it’s breaking the lock, jamming the tumblers, and then acting like it didn’t do anything. The data’s not speculative-it’s in the bloodwork, the platelet tests, the stent clot rates. We’re not talking about theoretical risk here. We’re talking about people who took their pills exactly as told… and still had another heart attack because their doctor didn’t know the difference between a PPI and a paperweight.
And yet, we still let pharmacists slap omeprazole on prescriptions like it’s aspirin. It’s not just negligence-it’s systemic laziness. Why aren’t hospitals running CYP2C19 tests on every post-stent patient? Why is this still a ‘maybe’ instead of a ‘hell no’?
Abigail Jubb
November 4, 2025 AT 21:47Oh, so now we’re diagnosing people based on their liver enzymes? Next they’ll be testing your soul for serotonin levels before prescribing antidepressants. I mean, really. If you’re taking clopidogrel, you’re already at high risk. Adding a PPI? That’s just common sense. Why are we turning every drug interaction into a genetic drama? People have been taking omeprazole with clopidogrel for decades and still live to retire. Maybe the real problem is overmedication, not enzyme inhibition.
Hope NewYork
November 6, 2025 AT 21:41so like… if you take omeprazole once a week for a bad pizza night, does it still ruin clopidogrel? bc i did that last month and my chest feels fine. also why do doctors act like we’re dumb? they just say ‘switch ppi’ like its magic. but pantoprazole costs 3x more and my insurance hates me. also, is this why my uncle died after his stent? he was on prilosec. i think the pharma companies are hiding something.
Bonnie Sanders Bartlett
November 8, 2025 AT 02:40I’ve seen this happen in my husband’s cardiology clinic. A patient came in with a recurrent clot after a stent. Turned out he’d been on omeprazole for years for ‘just a little acid.’ No one ever asked. No one ever checked. We switched him to pantoprazole and famotidine at night, and his platelet tests improved in six weeks. It’s not complicated. It’s just that doctors are busy, and patients don’t know to ask. So if you’re on clopidogrel, just ask your doctor: ‘Is my heartburn medicine safe with this?’ It’s a five-minute conversation that could save your life.
Melissa Delong
November 9, 2025 AT 20:14This entire post is a pharmaceutical industry scare tactic. The FDA doesn’t ban omeprazole because they know it’s dangerous-they ban it because they’re paid off. The COGENT trial was suppressed. The FAST-MI data was cherry-picked. And now they want you to believe you need genetic testing just to take heartburn medicine? That’s how they lock you into expensive brand-name drugs. Prasugrel? Ticagrelor? Those are 10x more expensive. They don’t care about your health-they care about your co-pay. Don’t fall for it.
Marshall Washick
November 10, 2025 AT 01:28I’ve sat with patients who’ve had two heart attacks because they didn’t know this interaction existed. One man, 58, took omeprazole daily since his first stent-his doctor never mentioned it. He didn’t even know what CYP2C19 was. When we switched him to pantoprazole, his platelet reactivity dropped from 85% to 38%. He cried. Not because he was scared-but because he finally felt like someone had listened. This isn’t just pharmacology. It’s about dignity. It’s about being treated like a person, not a data point. If your doctor doesn’t bring this up, ask. Don’t wait for a second event.
Abha Nakra
November 11, 2025 AT 08:34I work in a hospital in Mumbai where most patients can’t afford brand-name drugs. We see this interaction all the time. Omeprazole is cheap, widely available, and people take it for years. We’ve started using pantoprazole as our default when clopidogrel is involved-even though it costs a little more. The difference in outcomes is real. We don’t have genetic testing here, but we don’t need it. The rule is simple: if you’re on clopidogrel, avoid omeprazole and esomeprazole. That’s it. No complex science needed. Just common sense and a little care.
Neal Burton
November 12, 2025 AT 09:29Let’s be honest-this whole thing is a distraction. The real issue is that clopidogrel is a flawed, outdated drug. It’s a band-aid on a broken system. Why are we still relying on a prodrug that depends on a single enzyme that 25% of the population can’t even use properly? Why aren’t we pushing for universal access to ticagrelor or prasugrel? Why are we still playing genetic roulette with a 50-year-old drug? The PPI interaction is just a symptom. The disease is our entire approach to cardiovascular medicine: reactive, fragmented, and obsessed with cost over care.