What if your pain isn’t telling you that something’s broken?
Most people think pain means damage. If your back hurts, your spine must be worn out. If your knee aches, the cartilage is gone. That’s what doctors used to tell us. And for a long time, we believed it. But science has changed the game. Pain neuroscience education isn’t about fixing your body-it’s about changing how your brain interprets what’s happening inside it.
Think of pain like a smoke alarm. It’s not designed to detect fire. It’s designed to detect potential danger-and it gets overly sensitive over time. That’s what happens in chronic pain. Your nervous system doesn’t need tissue damage to keep sounding the alarm. It just needs to feel threatened. And that threat can come from stress, fear, sleep loss, or even past experiences. Pain neuroscience education helps you see this clearly.
How pain really works (no medical jargon)
Your brain doesn’t have a pain center. There’s no single switch that flips when you twist your ankle. Instead, pain is an output-a protective response your brain creates based on dozens of inputs. Nerve signals from your knee? Sure, they matter. But so does your mood, your beliefs, your sleep, your memories of past injuries, and whether you trust your doctor.
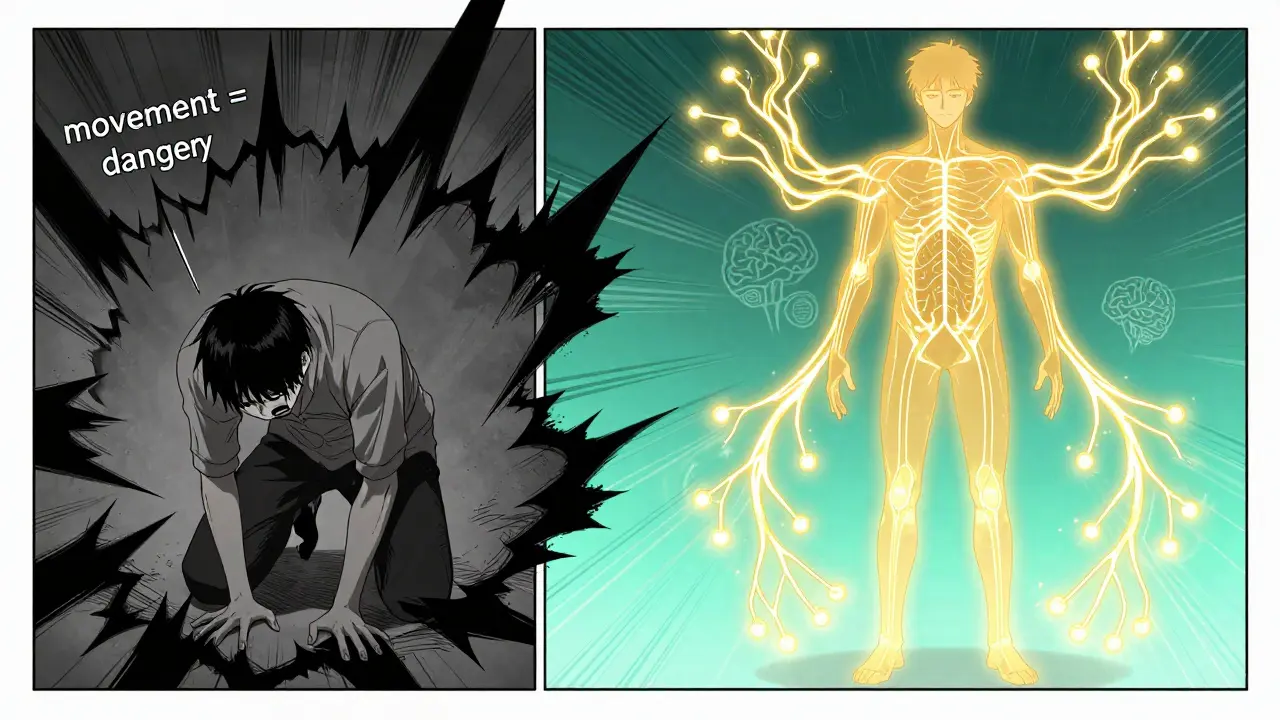
When you hurt your back lifting a box, your body sends signals to your brain. Normally, your brain says, “Got it. Rest for a bit.” Then it turns the alarm off after a few days. But in chronic pain, the brain keeps the alarm on-even after the tissue healed. Why? Because it learned to be scared. It thinks movement = danger. That’s not weakness. That’s biology.
This is where traditional pain advice fails. “Avoid activities that hurt” sounds logical. But if you stop moving because you’re scared, your muscles weaken. Your nerves get more sensitive. Your brain gets better at making pain. It’s a loop. Pain neuroscience education breaks that loop by teaching you: hurt doesn’t equal harm.
The science behind why education changes pain
Studies show that just learning about how pain works can reduce pain intensity by 1.7 to 1.8 points on a 10-point scale. That’s not magic. That’s neurobiology. When you understand that your pain isn’t a sign of damage, your brain starts to relax its defenses.
Brain scans confirm this. After pain neuroscience education, the part of the brain that sounds the alarm-the insula and amygdala-shows 22% less activity. Meanwhile, the prefrontal cortex, which helps you think clearly and make decisions, gets stronger. You’re not ignoring the pain. You’re rewiring your response to it.
One 2023 review of 23 clinical trials found that people who received pain neuroscience education had:
- 1.8-point drop in pain intensity (on a 0-10 scale)
- 12.3% reduction in disability
- 6.2-point drop in pain catastrophizing (thinking “this will never end” or “I can’t handle it”)
And here’s the kicker: when you combine this education with movement, the results jump by 30-40%. It’s not either/or. It’s both. Learn how pain works, then move safely. Your brain starts trusting movement again.
What pain neuroscience education actually looks like
It’s not a lecture. It’s a conversation. A good session lasts 30 to 45 minutes. The therapist doesn’t hand you a pamphlet. They use stories, metaphors, and visuals to make the science stick.
One common metaphor is the “sensitive smoke alarm.” Imagine your nervous system is like a smoke alarm set too close to the kitchen. Every time you toast bread, it goes off. You don’t need a fire. You just need a little smoke. That’s what chronic pain is. The alarm is hypersensitive. The goal isn’t to fix the alarm. It’s to teach you it’s not broken-it’s just overly cautious.
Another popular tool is the “pain neuromatrix.” Think of your brain as a network of pathways that constantly monitor your body, your emotions, your environment. Pain is the output of that whole system-not just your injured knee. This helps people stop blaming their spine, their disc, or their joint. They start seeing pain as a product of their whole life, not just their anatomy.
Most sessions include:
- Explaining peripheral and central sensitization (how nerves get louder over time)
- Introducing neuroplasticity (your brain can rewire itself)
- Linking stress, sleep, and pain
- Reframing fear-avoidance behaviors
These aren’t abstract ideas. They’re tools. And they work. A 42-year-old nurse with fibromyalgia reduced her daily pain meds from six pills to one every three days after six sessions of pain neuroscience education paired with graded activity. She didn’t get “cured.” She got her life back.
Who benefits-and who doesn’t
Pain neuroscience education works best for chronic pain: back pain, neck pain, fibromyalgia, complex regional pain syndrome, chronic headaches. In 82% of studies, it helped people with pain lasting longer than three months.
It doesn’t work as well for acute pain. If you just had surgery or broke a bone, your pain is likely signaling real tissue damage. In those cases, pain neuroscience education can still help reduce fear and improve recovery-but it’s not the main tool.
It also struggles with people who have severe cognitive impairment or low health literacy. If someone can’t follow a story about how the brain works, simple language and visuals are key. Some therapists switch from “neuroscience” to “pain biology” to make it feel less intimidating.
And here’s a hard truth: it doesn’t work if you’re expecting the pain to disappear overnight. This isn’t a quick fix. It’s a shift in perspective. People who quit after two sessions often say, “It didn’t help.” But those who stick with it for four to six sessions report life-changing results.
Why most clinics still don’t do this well
Despite strong evidence, only 28% of physical therapists in the U.S. feel confident delivering pain neuroscience education. Why? Time. Training. And old habits.
Many clinicians were taught to treat pain like a mechanical problem: “weak muscles,” “misaligned pelvis,” “tight hamstrings.” Changing that mindset takes effort. It means unlearning decades of biomedical training.
Plus, insurance doesn’t always pay for education. But since 2021, Medicare has started reimbursing pain neuroscience education under physical therapy codes (CPT 97160-97164). That’s changing things slowly.
And then there’s patient resistance. Some people say, “I just want you to fix my back.” When you tell them their back isn’t broken, they feel dismissed. That’s why skilled practitioners don’t say, “Your pain isn’t real.” They say, “Your pain is real-but it’s not telling you what you think it is.”
How to get started-with or without a therapist
You don’t need to wait for a referral. You can start today.
If you have a therapist, ask: “Have you been trained in pain neuroscience education?” If they haven’t, ask for resources. The Explain Pain handbook by David Butler and Lorimer Moseley is the gold standard. It’s written for patients, not just clinicians.
There are also apps. The Pain Revolution app has over 186,000 downloads. It breaks down pain science in short videos you can watch on your phone. One user in Adelaide said: “I watched it while waiting for my kid’s soccer practice. I didn’t even realize I was learning.”
Or try this simple exercise: Next time you feel pain, pause. Ask yourself:
- What’s happening in my life right now? (Stressed? Sleep-deprived? Sad?)
- Am I avoiding movement because I’m scared?
- Could this pain be my brain being overprotective?
That’s the first step of pain neuroscience education. You’re not fighting the pain. You’re getting curious about it.

The future of pain care
Researchers are now testing virtual reality versions of pain neuroscience education. Early results show people retain 30% more information with VR than with books or videos. Why? Because they’re not just hearing about it-they’re experiencing it.
Meanwhile, companies like Liberty Mutual are using pain neuroscience principles in workplace injury programs. Result? Workers’ compensation claims are 22% shorter. That’s not just better for employees-it’s better for businesses.
The big shift? We’re moving from “fix the body” to “retrain the brain.” And the evidence is clear: understanding pain is one of the most powerful tools we have for reducing it.
Real stories, real change
On Reddit, a user named PainWarrior87 wrote: “After six months of fearing movement would damage my back, the metaphor of a sensitive smoke alarm helped me understand my pain wasn’t signaling danger. I’ve since returned to hiking and reduced opioid use by 75%.”
That’s not a miracle. That’s neuroscience.
Pain neuroscience education doesn’t promise a pain-free life. It promises a life where pain doesn’t control you. Where you can move without fear. Where you can sleep without dread. Where you stop seeing yourself as broken-and start seeing yourself as capable.
That’s worth learning.
Is pain neuroscience education just for back pain?
No. While it’s most commonly used for chronic low back pain, it works for any persistent pain condition-neck pain, fibromyalgia, chronic headaches, joint pain, and even complex regional pain syndrome. The core idea-that pain is a protective output of the brain-is the same no matter where it’s felt.
Can I do pain neuroscience education on my own?
Yes, but it’s more effective with guidance. Books like Explain Pain and apps like Pain Revolution are great starting points. But working with a trained clinician helps you apply the concepts to your specific situation. They can spot fear-avoidance patterns you might miss and help you link understanding to movement safely.
Does pain neuroscience education mean my pain isn’t real?
Absolutely not. Your pain is real. Pain neuroscience education doesn’t deny your experience-it explains why it persists even when there’s no tissue damage. It’s like understanding why a car alarm goes off when someone walks by. The alarm isn’t broken. It’s just too sensitive. Your pain is the same.
How long does it take to see results?
Some people feel a shift after one session. But real change usually takes 4 to 6 sessions. The goal isn’t to eliminate pain quickly-it’s to change your relationship with it. That takes time. Most studies show the biggest improvements happen after 3 to 6 weeks of consistent understanding and movement.
Is pain neuroscience education covered by insurance?
In the U.S., Medicare and many private insurers now cover it under physical therapy codes (CPT 97160-97164) since 2021. In Australia, coverage varies by private health fund-some include it under allied health services. Always check with your provider, but don’t assume it’s not covered just because it’s education.
What’s the difference between pain neuroscience education and cognitive behavioral therapy (CBT)?
CBT focuses on changing thoughts and behaviors around pain. Pain neuroscience education focuses on changing your understanding of pain itself. They’re complementary. CBT helps you cope. Pain neuroscience education helps you reframe why you’re in pain. Many clinics now combine both. One study found 68% patient satisfaction with pain neuroscience education vs. 62% with CBT alone.
What to do next
If you’ve been living with chronic pain and feel stuck, don’t wait for a miracle cure. Start by learning. Grab the Explain Pain handbook. Watch a few videos from the Pain Revolution app. Ask your physiotherapist if they use pain neuroscience education. If they don’t, ask why. You deserve to understand your pain-not just endure it.
Change doesn’t happen in one session. But it does happen-when you stop seeing your body as broken and start seeing it as smart, adaptive, and capable of change. That’s the power of pain neuroscience education.


Herman Rousseau
December 21, 2025 AT 22:42Johnnie R. Bailey
December 22, 2025 AT 02:28Vikrant Sura
December 22, 2025 AT 07:36Ajay Brahmandam
December 22, 2025 AT 14:15Tarun Sharma
December 23, 2025 AT 16:18Aliyu Sani
December 24, 2025 AT 09:56Gabriella da Silva Mendes
December 25, 2025 AT 18:26Jim Brown
December 26, 2025 AT 22:00Sam Black
December 27, 2025 AT 01:36Jamison Kissh
December 28, 2025 AT 07:00Tony Du bled
December 29, 2025 AT 12:11Art Van Gelder
December 30, 2025 AT 07:45Kathryn Weymouth
December 31, 2025 AT 09:23Nader Bsyouni
January 1, 2026 AT 17:05Julie Chavassieux
January 3, 2026 AT 02:35