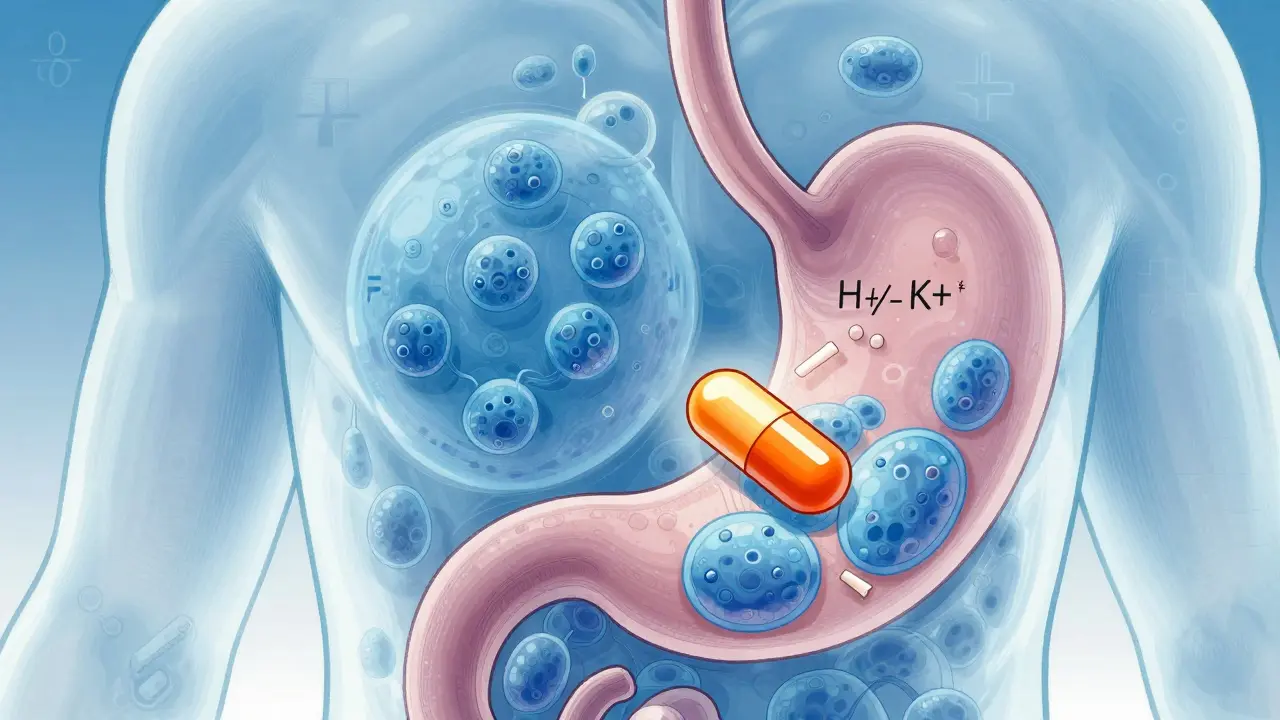
Proton Pump Inhibitors are medications that reduce stomach acid by blocking the H+/K+ ATPase enzyme system in stomach cells. They're commonly prescribed for heartburn, GERD, and ulcers. Over 15 million Americans take these drugs daily, but many don't realize the risks of long-term use. This article explains exactly when to stop PPIs and how to do it safely.
What Are Proton Pump Inhibitors?
Omeprazole is the first proton pump inhibitor approved by the FDA in 1989, commonly sold as Prilosec. It works by irreversibly blocking acid-producing pumps in stomach cells. Other common PPIs include Esomeprazole (Nexium), which is 30% more potent than omeprazole and requires once-daily dosing. These medications take 1-4 days to reach full effect, making them unsuitable for immediate heartburn relief. Unlike antacids or H2 blockers like famotidine (Pepcid), PPIs suppress acid production at the source.
Common Uses for PPIs
PPIs are most effective for Gastroesophageal Reflux Disease (GERD) with erosive esophagitis, where they heal damaged tissue in 90% of cases within 8 weeks. They're also used for peptic ulcers, Zollinger-Ellison syndrome, and preventing NSAID-induced ulcers. However, the American College of Gastroenterology found 70% of patients take PPIs without clear medical need, often for occasional heartburn that could be managed with lifestyle changes or antacids.
Long-Term Risks You Need to Know
A 2017 study in PMC showed Hip Fracture Risk increases by 42% after 4 years of PPI use and 55% after 6-8 years. This risk disappears within 2 years of stopping the medication. Hypomagnesemia (low magnesium) affects 0.5-1% of long-term users, causing muscle cramps, irregular heartbeat, and seizures. The FDA requires doctors to check magnesium levels in patients taking PPIs for over a year. Clostridium difficile infection risk rises 1.7-2.0 times with PPI use, especially in hospitals. This bacteria causes severe diarrhea and colon damage.
Vitamin B12 deficiency occurs in 10-15% of users after 2+ years of PPIs, leading to nerve damage and anemia. While some studies link PPIs to dementia or kidney disease, higher-quality research shows inconsistent evidence. The FDA's 2022 update confirmed magnesium deficiency as a serious risk, requiring clearer labeling on all PPI packaging.

When to Stop Taking PPIs
Follow the American Gastroenterological Association guidelines: stop PPIs if you've used them for more than 4-8 weeks for mild GERD without endoscopic confirmation of tissue damage. If you're taking over-the-counter PPIs for longer than 14 days without consulting a doctor, you're likely overusing them. The FDA explicitly warns against using OTC PPIs for more than 14 days every 3 months. For prescription PPIs, reassess need every 6-12 months. If your symptoms are manageable with lifestyle changes or occasional antacids, you probably don't need daily medication.
How to Stop Safely (Without Rebound Heartburn)
Stopping PPIs cold turkey causes Rebound Acid Hypersecretion in 40-80% of users. This temporary increase in stomach acid can worsen heartburn for 2-4 weeks. To avoid this:
- Reduce your dose by half for 1-2 weeks (e.g., 20mg daily → 10mg daily).
- Switch to taking the reduced dose every other day for 1-2 weeks.
- Use antacids or H2 blockers like famotidine only when symptoms occur.
- Consult your doctor before stopping completely, especially if you have a history of ulcers or Barrett's esophagus.

Alternatives to Daily PPI Use
For occasional heartburn, Antacids like Tums or Maalox provide immediate relief and carry no long-term risks. H2 Blockers such as famotidine (Pepcid) or ranitidine (Zantac) are 30-50% less effective than PPIs for severe GERD but safer for short-term use. Lifestyle changes work wonders: lose weight if overweight, avoid trigger foods (coffee, spicy meals), eat smaller dinners, and don't lie down for 3 hours after eating. Elevating the head of your bed by 6 inches reduces nighttime reflux by 70%.
Frequently Asked Questions
Can I stop PPIs cold turkey?
No. Stopping abruptly causes severe rebound heartburn in most people. Always taper under medical supervision. The American College of Gastroenterology recommends reducing dose gradually over 2-4 weeks.
What are the signs of magnesium deficiency from PPIs?
Symptoms include muscle cramps, tremors, fatigue, irregular heartbeat, and seizures. If you experience these while on PPIs for over a year, get your magnesium levels checked immediately. The FDA requires healthcare providers to monitor this in long-term users.
Are over-the-counter PPIs safer than prescription ones?
No. OTC PPIs like Prilosec OTC have the same risks as prescription versions. The FDA mandates OTC labels warn against use beyond 14 days without a doctor's advice. Many people unknowingly exceed this limit, increasing long-term risks.
Can PPIs cause kidney damage?
The FDA issued a warning in 2016 about acute interstitial nephritis (a type of kidney inflammation) linked to PPIs. However, progression to chronic kidney disease is rare and usually reversible if caught early. Regular kidney function tests are recommended for long-term users.
What's the best way to manage heartburn without PPIs?
For mild cases, try antacids for immediate relief and H2 blockers like Pepcid for ongoing management. Lifestyle changes are crucial: avoid eating 3 hours before bed, skip caffeine/alcohol, lose excess weight, and sleep with your head elevated. Studies show these reduce reflux symptoms by 60-80% in most people.

Elliot Alejo
February 5, 2026 AT 17:24I've been on PPIs for a few years and never realized the risks until reading this. The part about magnesium deficiency was eye-opening.
It's important to taper off properly instead of stopping cold turkey.
I'll definitely consult my doctor before making any changes.
Cullen Bausman
February 7, 2026 AT 01:53This is a critical issue for all citizens
Pharmaceutical companies profit from overprescribing
The FDA needs to act immediately
People are getting sick because of unnecessary prescriptions
It's a national health crisis
Diana Phe
February 7, 2026 AT 07:05This is all a big pharma scam
They want us dependent on PPIs to keep profits up
The FDA is in cahoots with them
They downplay the risks
I read that PPIs cause cancer
They're hiding that
Don't trust the system
Nancy Maneely
February 8, 2026 AT 04:32omg this is so important! i had no idea about the hip fracture risk
ppis are basically a ticking time bomb for seniors
the FDA needs to wake up
people are dying because of this
this article should be mandatory reading for every doctor
#yikes
Katharine Meiler
February 8, 2026 AT 12:05As a healthcare professional, I appreciate the thorough breakdown of PPI risks presented in this article.
The evidence regarding magnesium deficiency is particularly robust, with multiple studies showing a clear correlation between long-term PPI use and hypomagnesemia.
This condition can lead to serious complications such as muscle cramps, arrhythmias, and even seizures if left untreated.
Interestingly, the FDA has recently updated its labeling requirements to highlight this risk more prominently.
While some studies have suggested a potential link between PPIs and dementia or kidney disease, the current consensus from higher-quality research indicates inconsistent evidence.
It's important to note that the risk of Clostridium difficile infection increases significantly with PPI use, especially in hospital settings.
For patients with Barrett's esophagus or severe erosive esophagitis, PPIs remain essential.
However, for those using OTC PPIs for occasional heartburn, lifestyle modifications should be the first line of defense.
Proper tapering protocols are absolutely critical to avoid rebound acid hypersecretion.
Many patients stop PPIs abruptly without guidance, leading to severe symptoms.
I recommend regular monitoring of magnesium levels in patients on long-term therapy.
Additionally, the American Gastroenterological Association guidelines clearly state that PPIs should be used at the lowest effective dose for the shortest duration possible.
It's also worth mentioning that the risk of hip fracture is most pronounced in older adults with prolonged use.
Finally, healthcare providers should regularly reassess the necessity of PPI therapy every 6-12 months.
Overall, this article does an excellent job of highlighting both the benefits and risks of these commonly prescribed medications.
Joyce cuypers
February 8, 2026 AT 23:49great info katharine!
i'll share this with my patients
must remember to taper slowly
thanks for the tips on alternatives 😊
Lana Younis
February 10, 2026 AT 10:38This is such important info! I love how it breaks down the risks clearly.
For folks from different backgrounds, it's crucial to know that lifestyle changes can really help.
Like avoiding spicy food at night or elevating the head of the bed.
Thanks for sharing this so clearly!
Samantha Beye
February 10, 2026 AT 22:20This is crucial information.
Andre Shaw
February 11, 2026 AT 21:43Actually, most of these risks are exaggerated.
PPIs are safe when used correctly.
The real issue is doctors not monitoring patients.
The FDA's warnings are overblown.
I've been on them for years with no issues.
Stop fearmongering.
one hamzah
February 12, 2026 AT 21:59This is super helpful! 🌟
I'm from India and PPIs are commonly prescribed here too.
The magnesium deficiency part is crucial.
People should get their levels checked.
Thanks for sharing! 🙌