Most people know psoriasis as the red, scaly patches on the skin. But for about 1 in 3 people with psoriasis, the problem doesn’t stop at the skin. It creeps into the joints - causing pain, swelling, and sometimes permanent damage. This is psoriatic arthritis (PsA), a hidden complication that often goes undiagnosed until it’s too late.
It’s Not Just Skin Deep
Psoriatic arthritis isn’t a side effect of psoriasis. It’s a separate autoimmune disease that happens to share the same root cause: your immune system turns on your own body. In psoriasis, it attacks skin cells. In psoriatic arthritis, it attacks the joints, tendons, and even the places where tendons attach to bone. This is why someone can have flaky elbows and swollen fingers at the same time - it’s the same storm, hitting different parts of the body.The connection isn’t random. About 30% of people with psoriasis will develop joint symptoms. For most, the skin comes first - usually 5 to 10 years before the joints start acting up. But in 15% of cases, the joints hurt before the skin shows any sign. That’s when things get tricky. Many patients see their doctor for stiff knees or achy fingers and get told it’s just aging, or maybe a sports injury. By the time the skin patches appear, the damage is already done.
What Does Psoriatic Arthritis Actually Feel Like?
The pain isn’t like the dull ache of osteoarthritis. It’s sharp, stiff, and worse in the morning or after sitting still. You might wake up feeling like your hands are glued shut. That’s not just normal stiffness - it’s inflammation. About 92% of people with PsA report this kind of morning tightness.One of the most telling signs is dactylitis - when an entire finger or toe swells up like a sausage. It’s not just the joint. It’s the whole digit, inflamed from tip to base. Around half of people with PsA get this. It’s so distinctive that doctors use it as a diagnostic clue.
Then there’s enthesitis - inflammation where tendons or ligaments meet bone. Think of your Achilles tendon or the bottom of your foot. If you’ve ever had heel pain that doesn’t go away with rest, it might not be plantar fasciitis. It could be PsA. About 28% of patients have Achilles tendon involvement. Another 22% feel it in the soles of their feet.
Nails are another big clue. If you’ve got pitted fingernails, or your nails are lifting from the bed, or turning yellow, that’s not just bad hygiene. Eighty percent of PsA patients with nail changes have the condition. And if you see nail pitting along with swollen toes, there’s an 89% chance it’s psoriatic arthritis.
Five Ways PsA Shows Up in the Body
PsA doesn’t look the same in everyone. It splits into five main patterns:- Asymmetric oligoarthritis - the most common. It hits 35-40% of people. One knee, one wrist, maybe a finger on the left hand. No symmetry. Just random joints acting up.
- Symmetric polyarthritis - affects 25-30%. Looks like rheumatoid arthritis because it hits matching joints on both sides. But unlike RA, it rarely causes high levels of rheumatoid factor in the blood.
- Distal interphalangeal predominant (DIP) - 25% of cases. Only the joints right under the nails get damaged. This one is almost unique to PsA. If your fingertips are swollen and your nails are pitted, this is likely the culprit.
- Spondylarthritis - 5-10%. This one targets the spine and lower back. Pain gets worse when you sit still, better when you move. People mistake it for a bad back. But if you also have psoriasis or nail changes, it’s PsA.
- Arthritis mutilans - less than 5%. The rarest and most destructive. Bones dissolve. Fingers shorten. You get what’s called an “opera glass hand” - where the fingers collapse inward. It’s devastating, but thankfully uncommon.

How Is It Different From Other Arthritis?
People confuse PsA with rheumatoid arthritis (RA) or osteoarthritis (OA). But they’re not the same.RA hits joints symmetrically - both wrists, both knees. PsA? Often asymmetric. RA also shows up with a positive rheumatoid factor blood test. PsA? Negative. Always.
OA is just wear and tear. It’s common in older adults. It doesn’t cause swelling, redness, or morning stiffness that lasts over an hour. PsA does. And unlike OA, PsA can affect your eyes (uveitis), your gut (inflammatory bowel disease), and even your heart.
X-rays tell the story too. In PsA, you might see “pencil-in-cup” deformities - where one bone wears down into another like a pencil tip fitting into a cup. You might also see new bone growth around tendons - called “whiskering.” That’s something OA never does.
Why Diagnosis Takes So Long - And Why It Matters
The average person waits 2 to 5 years to get a correct diagnosis. Over 40% see three or more doctors before someone connects the dots. Why? Because doctors aren’t always looking for it. A dermatologist sees the skin. A rheumatologist sees the joint. But no one puts them together.That delay costs you. A study from Toronto found that if you wait more than 12 months to get treated, you’re 3.2 times more likely to have permanent joint damage within five years. Every month counts.
Early signs? Stiffness that won’t go away. Fatigue that makes you cancel plans. Nail changes. Even if you don’t have skin lesions yet, these are red flags.
What Works - And What Doesn’t
Treatment has improved dramatically. The goal now isn’t just to manage pain. It’s to stop the disease in its tracks.First-line drugs? Methotrexate. Used in 65% of new cases. But it doesn’t work for everyone. If it fails, biologics come in - drugs that target specific parts of the immune system.
TNF inhibitors (like adalimumab or etanercept) help 65% of patients reach minimal disease activity within six months. Newer drugs - IL-17 and IL-23 inhibitors - are even better. One study showed guselkumab (an IL-23 blocker) helped 64% of patients achieve a 50% improvement in symptoms at just 24 weeks.
But here’s the catch: 30% of people don’t respond to their first biologic. That’s why treatment is personal. Your doctor may need to try a few before finding the right one.
There are risks too. JAK inhibitors - newer oral drugs - carry a higher chance of heart problems and cancer. The FDA requires special monitoring for them. That’s why treatment isn’t one-size-fits-all.
What Triggers Flares - And How to Avoid Them
PsA doesn’t flare for no reason. Patients report clear triggers:- Stress - cited by 85%
- Infections - especially strep throat - 63%
- Cold weather - 57%
- Obesity - if your BMI is over 30, your risk of PsA jumps 2.3 times
- Joint injury - trauma to a joint can trigger PsA in that exact spot - risk goes up 4.1 times
Managing these doesn’t cure PsA, but it helps. Lose weight. Avoid infections. Manage stress. Stay warm in winter. These aren’t just lifestyle tips - they’re part of your treatment plan.
Why You Need Two Doctors, Not One
PsA lives at the intersection of skin and joints. That means you need both a dermatologist and a rheumatologist working together. Studies show that when they do, 82% of patients get optimal outcomes. When they don’t? Only 54%.That’s why integrated care matters. Your skin doctor should be talking to your joint doctor. Your nail changes should be documented in your rheumatology chart. Your joint pain should be noted in your dermatology notes.
Tools like the NAPSI (Nail Psoriasis Severity Index) and MASES (for enthesitis) help both doctors track progress the same way. No more guessing. Just data.
What’s Next?
The future is personal. By 2027, doctors expect to use your genes and blood proteins to pick the best drug for you - not guess. Clinical trials are already testing new drugs that target the JAK-STAT pathway and other immune signals.But right now, the most powerful tool you have is awareness. If you have psoriasis and your joints ache, don’t wait. Don’t assume it’s just aging. Don’t let another doctor miss the signs. Bring up PsA. Ask for a referral. Get your nails checked. Get an X-ray if needed.
Psoriatic arthritis doesn’t care how young you are. It doesn’t care if your skin looks fine today. It’s waiting for the right moment to strike. The earlier you catch it, the more of your body you keep.
Can you have psoriatic arthritis without psoriasis?
Yes, but it’s rare. About 15% of people develop joint symptoms before any skin patches appear. This makes diagnosis harder, because doctors don’t always connect joint pain to psoriasis. If you have nail changes, dactylitis, or enthesitis - even without visible skin psoriasis - you should still be tested for PsA.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis (RA) typically affects joints symmetrically - both hands, both knees - and shows up with a positive rheumatoid factor blood test. Psoriatic arthritis is often asymmetric, rarely has a positive rheumatoid factor, and is linked to skin and nail changes. X-rays also show different patterns: PsA can cause new bone growth and pencil-in-cup deformities, which RA doesn’t.
Does psoriatic arthritis show up on X-rays?
Yes, especially in later stages. Early on, X-rays might look normal. But as the disease progresses, you’ll see signs like joint erosion, new bone formation at tendon attachments (called periostitis), and the unique “pencil-in-cup” deformity. Ultrasound and MRI are even better for catching early inflammation before it shows on X-rays.
Can psoriatic arthritis be cured?
There’s no cure yet. But with early treatment, many people reach “minimal disease activity” - meaning symptoms are barely noticeable, and joint damage stops progressing. Some even go into remission. The goal isn’t to eliminate the disease, but to control it so it doesn’t control your life.
What happens if psoriatic arthritis is left untreated?
Untreated PsA causes irreversible joint damage. Over time, bones erode, tendons pull away, and deformities form - like shortened fingers or fused joints. It also increases your risk of heart disease, diabetes, and depression. Studies show that people who wait more than a year to get treated are over three times more likely to have serious joint damage within five years.


Dina Santorelli
February 4, 2026 AT 19:00So I went to my dermatologist last year for a weird nail thing and she just said it was fungus. Two months later I couldn’t bend my pinky. Turns out it was PsA. No one connects the dots until it’s too late. I’m 31. This isn’t ‘just aging’.
Danielle Vila
February 5, 2026 AT 01:35EVERYONE knows Big Pharma doesn’t want you to know this - they make billions off methotrexate and biologics but if you just cut out gluten and do cold plunges daily, your immune system ‘resets’ and poof - PsA vanishes. I read it on a blog written by a guy who cured his Lyme with essential oils. Also, the government is hiding the truth about the ‘joint-destroying microwave frequency’ in city water. Check the comments on my YouTube video - I’ve got the X-rays.
Thorben Westerhuys
February 5, 2026 AT 05:37Okay, so I’ve got this… this… this *thing* in my heel that won’t go away. I’ve tried everything. Stretching. Ice. Massage. Nothing. Then I read this post. And I realized - it’s not plantar fasciitis. It’s enthesitis. I’m crying. I’ve been told I’m ‘just lazy’ for three years. This… this makes sense. Thank you.
Laissa Peixoto
February 5, 2026 AT 15:56There’s a deeper truth here that gets lost in the clinical language: PsA isn’t just a disease of the body - it’s a betrayal by your own biology. Your immune system, the very thing meant to protect you, becomes the enemy. And the worst part? You don’t get to choose when it turns. It doesn’t care if you’re healthy, young, or ‘good’ - it just… happens. That’s why awareness isn’t just medical - it’s existential. We’re all one misdiagnosed joint away from realizing how fragile we are.
Lana Younis
February 7, 2026 AT 06:16yo so i had this weird nail thing going on + swollen toe and i was like ‘nah, probably just my shoes’… then i saw a doc who actually knew what dactylitis was and was like ‘ohhh that’s psa’ - mind blown. i didn’t even know i had psoriasis cause my patches were so light. but my nails? totally pitted. anyway - if you got weird nail junk + joint pain? go get checked. no cap. your future self will thank you. also - see both docs. derm + rheum. they gotta talk. like, literally text each other. lol.
Samantha Beye
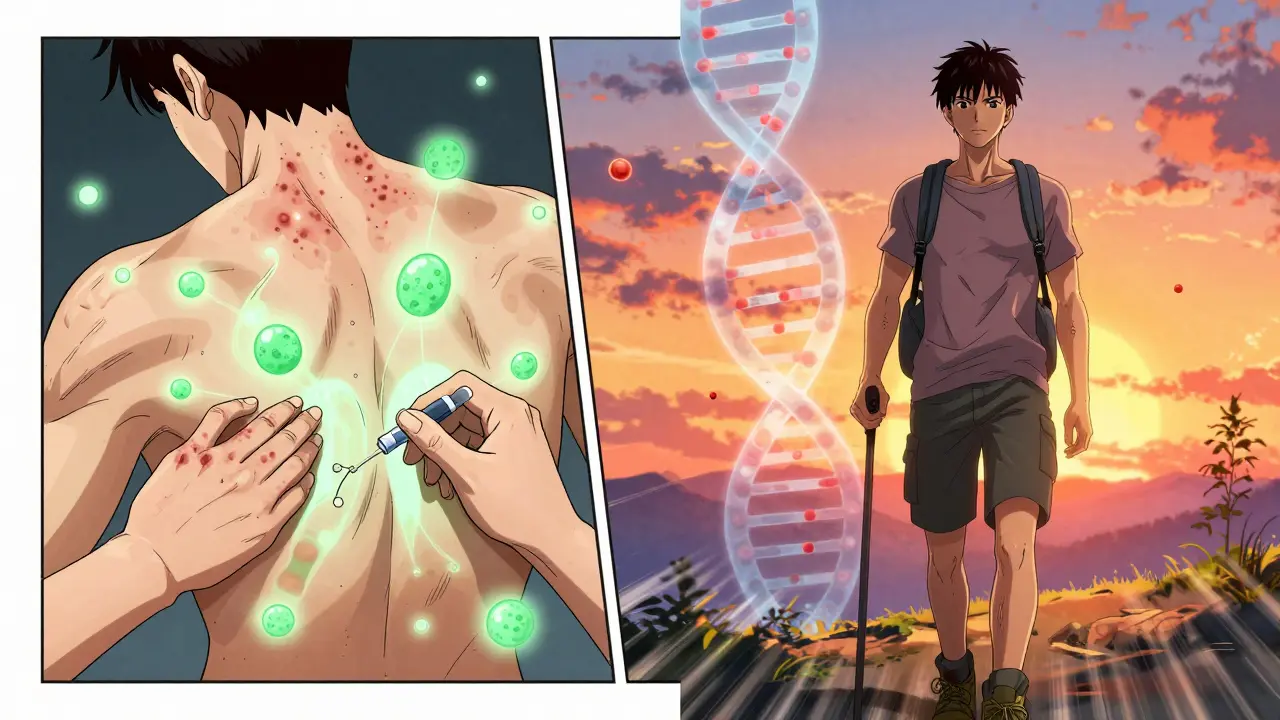
February 7, 2026 AT 21:44My brother was diagnosed last year. He’s 28. He thought it was gym injuries. He didn’t even know he had psoriasis until his wife pointed out the flakes on his scalp. Now he’s on a biologic. He’s back to hiking. He’s alive again. Don’t wait. Don’t normalize pain. You deserve to move without fear.
Rene Krikhaar
February 8, 2026 AT 11:17Jennifer Aronson
February 9, 2026 AT 14:17It is worth noting that the integration of dermatological and rheumatological care pathways significantly improves diagnostic accuracy and long-term outcomes, as evidenced by multiple peer-reviewed studies conducted across North American and European tertiary centers.