Medication Side Effect Risk Calculator
How It Works
This calculator estimates your risk of medication side effects based on the number and type of medications you take. Higher risk indicates greater potential need for remote monitoring tools.
Your Risk Assessment
Low Risk (10-25%)
Based on your inputs, your estimated risk of serious medication side effects is relatively low.
Consider monitoring for symptoms like dizziness or fatigue, but your risk of severe reactions appears minimal.
Your Risk Assessment
Moderate Risk (26-50%)
Monitoring for side effects could be beneficial based on your medication profile.
Consider using remote monitoring tools like Medisafe or Mango Health to detect early signs of adverse reactions.
Watch for symptoms like irregular heartbeats, confusion, or abnormal fatigue.
Your Risk Assessment
High Risk (51-75%)
Based on your medication profile, you're at significant risk for serious side effects.
Remote monitoring tools are highly recommended to detect adverse reactions early.
Consider discussing with your doctor whether you need monitoring for specific drugs like anticoagulants or antipsychotics.
How Remote Monitoring Can Help You
Tools like those mentioned in the article can detect:
- Changes in heart rate variability after medication
- Signs of drowsiness or tremors through facial recognition
- Abnormal patterns in your symptoms through AI analysis
Every year, over 1.3 million people in the U.S. end up in the emergency room because of bad reactions to their medications. Many of these reactions don’t show up until it’s too late-dizziness that leads to a fall, a心跳 that spikes overnight, or confusion mistaken for aging. What if you could catch these problems before they become emergencies? That’s exactly what remote monitoring for medication side effects is designed to do.
How It Works: More Than Just Pill Reminders
Early medication apps were simple: they buzzed your phone to remind you to take your pills. Today’s systems do far more. They watch your body as you take your meds. A smartwatch tracks your heart rate variability after you swallow a beta-blocker. Your phone’s camera notices if your eyelids droop too long after a sedative. An app asks you to type how you’re feeling-and then cross-references your words with thousands of known side effects from the FDA’s database. These aren’t sci-fi fantasies. They’re real tools used in clinics and homes right now. The core idea is simple: link medication intake with real-time physiological changes. If your heart rate drops 20% two hours after taking a new blood pressure drug, the system flags it. Not because it’s certain you’re having a reaction-but because it’s suspicious enough to warrant a call from your doctor.Top Platforms and What They Actually Do
Not all apps are built the same. Here’s what the leading platforms are actually doing in 2025:- Medisafe (v8.3): Integrates with 78 wearables, including Apple Watch and Fitbit. It doesn’t just remind you to take your pills-it watches for abnormal heart rate variability (HRV). If your HRV stays 15% below your personal baseline for two full days, it sends an alert to your care team. This threshold was tested in a 2024 study with Massachusetts General Hospital.
- AiCure: Uses your smartphone camera to confirm you swallowed your pill-96.7% accurately. It also analyzes your facial movements for signs of drowsiness, tremors, or slurred speech. Used mostly in clinical trials, it’s not meant for everyday use due to cost ($249/month per patient).
- Mango Health (v5.2.1): Reads what you type. If you say, “I feel foggy since I started this new antidepressant,” it matches your words to 1.2 million known side effect reports. It’s 89.3% accurate at spotting medication-related symptoms, according to a peer-reviewed study in the Journal of Medical Internet Research.
- HealthArc: Connects to 42 medical devices-glucometers, blood pressure cuffs, even oxygen sensors. Its Adaptive Side Effect Detection Engine (ASDE) finds patterns across 1,850+ drug-side effect combinations. But it’s complex. Clinics need nearly 15 hours of training just to use it well.
- Pill Identifier & Med Scanner (v2.3): Takes a photo of your pill and tells you what it is-94.6% accuracy across 15,000+ medications. But it doesn’t monitor your body. It’s great for avoiding mix-ups, useless for catching side effects.
Where These Tools Shine-and Where They Fail
The biggest win? Early detection. At Mayo Clinic, AI-driven monitoring cut severe drug reactions in heart failure patients by 37%. Patients on diuretics, who often develop dangerous electrolyte imbalances, now get alerts before their labs turn abnormal. But here’s the catch: these systems aren’t perfect. They get it wrong about 1 in 5 times. Fatigue from depression? The app thinks it’s a side effect of your antidepressant. A headache from stress? Flagged as a reaction to your migraine med. This “alert fatigue” is real. In a 2025 AMA survey, 68% of doctors admitted they turned off alerts because they were too noisy. And when you ignore the alarms, you might miss the one that matters. Another serious issue: bias. Preliminary data from the Centers for Medicare & Medicaid Services shows that elderly African American patients get 23% fewer alerts than white patients for the same symptoms. Why? The algorithms were trained mostly on data from younger, white populations. The FDA now requires all side effect detection tools to prove they work equally well across age, race, and gender-or they won’t get approval.
Who Benefits Most?
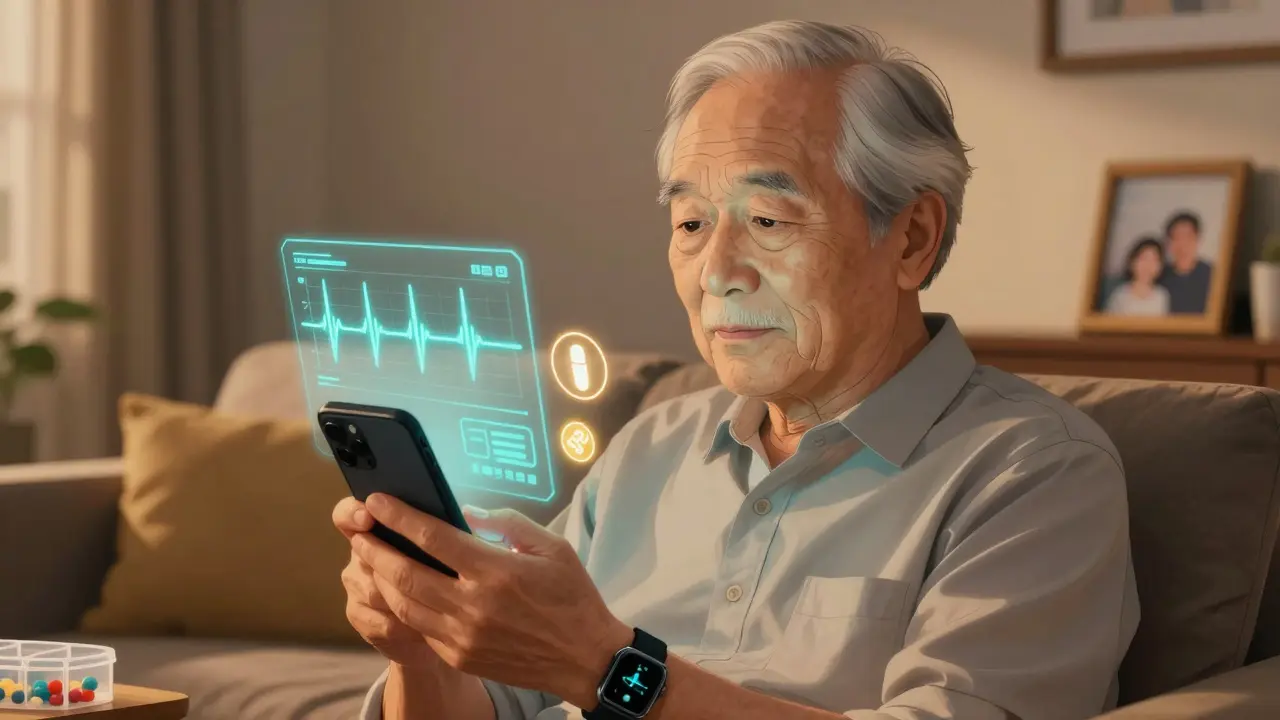
This isn’t for everyone. But for some, it’s life-changing:- People on multiple medications: Especially seniors taking 5+ drugs. A 2025 caregiver app called mySeniorCareHub flagged a dangerous interaction between a blood thinner and a common OTC painkiller-before the patient even took it.
- Patients on high-risk drugs: Anticoagulants, antipsychotics, chemotherapy agents, and heart rhythm drugs. These are the ones that can kill quietly.
- Those with chronic conditions: Diabetes, heart failure, epilepsy. Their meds need constant tuning. Remote monitoring gives doctors real-time data instead of waiting for a monthly visit.
What You Need to Get Started
You don’t need a hospital to use these tools. Many are available to individuals:- Device requirements: iPhone 11 or newer, Android 10+, 3GB+ RAM. Older phones struggle with the AI processing.
- Wearables: Apple Watch Series 5 or later, Fitbit Charge 6, or Garmin Vivosmart 5. These track HRV, sleep, and activity-key signals for side effects.
- Connectivity: Wi-Fi or cellular. For elderly users without reliable Wi-Fi, cellular-enabled devices like Medtronic’s CareLink system maintain 99.2% uptime.
- Integration: Most platforms sync with Epic, Cerner, and other EHRs through FHIR API. If your doctor uses one of these, they can see your data without you having to share it manually.
Cost, Reimbursement, and Privacy
Costs vary wildly. Medisafe charges healthcare providers $99 per patient per year. AiCure? $249 per month. Most patients don’t pay directly-their insurer or clinic does. Good news: Medicare and Medicaid now reimburse for Remote Therapeutic Monitoring (RTM) that includes side effect tracking. As of late 2024, providers can bill $52-$67 per patient per month for this service. That’s a game-changer for clinics. But privacy? That’s the elephant in the room. Your side effect data-mood swings, dizziness, heart irregularities-is deeply personal. Right now, HIPAA protects it, but only if your provider follows the rules. What if an insurer gets access? Could your premiums go up because your app flagged “possible depression” from a blood pressure med? A 2025 KLAS survey found 72% of patients are afraid of exactly that.The Future: Genetic Matching and Digital Twins
The next leap isn’t just about watching your body. It’s about understanding your genes. Mayo Clinic’s RIGHT Study combines genetic testing with remote monitoring. If your DNA shows you metabolize certain drugs slowly, the system adjusts alerts accordingly. In trials, this cut adverse events by 67%. AiCure is testing “Digital Twin” technology-creating a virtual model of how your body responds to meds based on your history, genetics, and real-time data. Early results show it predicts individual side effect risk 43% better than before. The FDA is tightening rules. By 2026, all AI-based side effect tools must prove they reduce false positives by 30-40%. That means fewer annoying alerts-and more trust in the ones that remain.Final Thoughts: A Tool, Not a Replacement
Remote monitoring won’t replace your doctor. It won’t diagnose you. But it can be the early warning system your body doesn’t have. If you’re on multiple meds, have a chronic illness, or care for someone who does-ask your provider if a side effect monitoring tool is right for you. Don’t assume it’s too high-tech. Most apps are designed for people who aren’t tech-savvy. The real question isn’t whether you can use it. It’s whether you can afford not to.The data is clear: these tools prevent hospitalizations. They save lives. But only if we use them wisely-and demand they work for everyone, not just some.

Peter Ronai
December 16, 2025 AT 17:33This is all just corporate snake oil dressed up as innovation. You think your smartwatch can tell if a beta-blocker is killing you? My grandma took three pills a day for 20 years and never needed an app to tell her when she felt like crap. These systems flag fatigue from depression as a drug side effect? That’s not AI-that’s lazy programming with a $99 subscription fee. And don’t get me started on the ‘digital twin’ nonsense. We’re not building avatars for our organs, we’re trying not to die from bad prescriptions.
And yes, I’ve read the Mayo Clinic study. It was funded by Medisafe’s parent company. Surprise, surprise-results look great when you cherry-pick your cohort. Real people? We’re getting alerts for sneezing and coffee jitters. I turned mine off. My doctor still has my chart. He’s not an algorithm.
Stop selling fear as healthcare. We don’t need more noise. We need better doctors, not more sensors watching us sweat.
Michael Whitaker
December 16, 2025 AT 23:41While I acknowledge the technical sophistication of these platforms, one must critically examine the epistemological foundations upon which they are predicated. The assumption that physiological data, when aggregated and algorithmically interpreted, yields clinically actionable insight is not only reductive-it is ontologically flawed. Human phenomenology-subjective experience, contextual stressors, cultural expressions of discomfort-is systematically erased in favor of quantifiable metrics that bear little resemblance to lived reality.
Moreover, the integration of such tools into EHRs via FHIR API, while ostensibly seamless, introduces a latent form of algorithmic paternalism. The physician’s clinical judgment becomes a rubber stamp for machine-generated alerts, thereby eroding the therapeutic alliance. One must ask: who is truly in control-the patient, the clinician, or the data pipeline?
And let us not overlook the ethical vacuum surrounding reimbursement structures. When Medicare pays $67/month for RTM, are we incentivizing care-or commodifying vulnerability?
Brooks Beveridge
December 17, 2025 AT 00:28Hey everyone-just wanted to say this stuff actually saved my mom’s life. She’s 78, on five meds, and her Medisafe app flagged a weird HRV dip two days after she started a new diuretic. She didn’t even feel different. But the alert went to her nurse, they checked her potassium, and it was dropping fast. They adjusted it before she ended up in the hospital.
I know it’s not perfect. I’ve seen false alarms too. But this isn’t about replacing doctors-it’s about giving them more eyes. And yeah, the bias stuff is real. We need better data. But throwing out the whole system because it’s not perfect? That’s like refusing to use seatbelts because they don’t prevent every crash.
If you’re on multiple meds, or caring for someone who is-try it. Talk to your doc. Ask if they’ve got a digital navigator. It’s not magic. But it’s a safety net. And sometimes? That’s all you need. 💙
Jigar shah
December 17, 2025 AT 20:04It is noteworthy that the precision of symptom detection varies significantly across platforms. For instance, AiCure’s 96.7% pill-swallowing accuracy is commendable, yet its reliance on facial movement analysis may be confounded by cultural variations in nonverbal expression. Furthermore, the training datasets referenced in the Journal of Medical Internet Research study appear to lack sufficient representation from non-Western populations, potentially limiting generalizability.
Additionally, the cost structure-particularly AiCure’s $249 monthly fee-raises questions regarding equity of access. While reimbursement via Medicare is a positive development, it remains unclear whether low-income or rural populations can meaningfully participate in these programs without institutional support.
Future iterations should prioritize open-source algorithms and community-driven data collection to mitigate algorithmic bias and ensure global applicability.
Joe Bartlett
December 18, 2025 AT 21:09UK’s got better ways. We’ve got NHS apps that just text you: ‘How you feeling?’ No fancy cameras. No $200 watches. Just a simple check-in. And guess what? It works. You don’t need AI to spot someone’s dizzy. Just ask them.
These US apps are overengineered. You’re paying for a fancy gadget to tell you what your GP could find in five minutes. Waste of cash. And don’t get me started on the privacy nightmares. Your heart rate data isn’t yours anymore-it’s owned by some Silicon Valley startup. Yikes.
Josh Potter
December 19, 2025 AT 15:45bro this is the future and you’re still stuck in 2010? 😭
my aunt’s on chemo and her HealthArc app told her to call her oncologist because her oxygen dipped after a new drug. She did. Turns out she had a tiny pulmonary embolism. They caught it before she collapsed. No one was yelling. No alarms. Just a quiet nudge.
and yeah, sometimes it’s wrong. So what? My phone autocorrects my typos too. I don’t trash the whole keyboard.
if you’re too lazy to set up an app, fine. But don’t act like people who use this are dumb. My grandma’s 80 and she uses it. She says it makes her feel safe. That’s worth more than your skepticism.
also-yes, the bias is real. but that’s not the tech’s fault. it’s the data’s fault. fix the data, not the tool. stop being a hater. 🙃
Jody Patrick
December 20, 2025 AT 23:14Another American tech fantasy. We don’t need sensors. We need cheaper drugs and better training for doctors. This is just more profit-driven noise. Stop selling fear. People are dying because they can’t afford insulin, not because their watch didn’t beep.
Also, why is every solution here American? No one else in the world needs this much tech to take pills. We’re not special. We’re just greedy.
Anna Giakoumakatou
December 21, 2025 AT 22:29Oh, so now my dizziness is a ‘side effect’ and not just… me being tired after caring for my three kids and working two jobs? How convenient. Let me just plug my Apple Watch into my emotional exhaustion and call it ‘AI-powered healthcare.’
And of course, the algorithm didn’t learn that elderly Black patients have different baseline vitals-it just assumed they’re fine because their data didn’t fit the white, middle-class, 40-year-old model. Classic.
At this point, I’d rather just Google my symptoms and pray. At least then I’m not paying $249/month to be told I’m ‘at risk’ because I yawned too much.
Donna Packard
December 23, 2025 AT 02:03I just wanted to say thank you for writing this. I’ve been scared to bring up monitoring tools with my dad-he’s 82, hates tech, thinks he’s fine. But after reading this, I’m going to ask his doctor about Medisafe. He’s on four meds and has had two falls in the last year. I don’t want to wait until something worse happens.
It’s not about being perfect. It’s about being present. And sometimes, a quiet alert is the only thing standing between a normal day and a hospital bed.
You’re right. It’s not a luxury. It’s a lifeline.
Patrick A. Ck. Trip
December 23, 2025 AT 15:08Thank you for this thoughtful, well-researched piece. I appreciate the nuance in acknowledging both the promise and the pitfalls of these systems.
I’m a caregiver for my wife, who has Parkinson’s and takes seven medications. We’ve been using Mango Health for six months. The alerts are sometimes overwhelming, but the one that caught her serotonin interaction with an OTC cold med? That was a miracle.
I do wish the interface was less glitchy-I keep accidentally logging ‘tired’ instead of ‘tremors’-but the fact that it connects to her neurologist’s system means she doesn’t have to repeat everything every visit.
Let’s not throw the baby out with the bathwater. The bias issue? We need to fix it. The cost? We need to push for universal access. But the potential? It’s real. And it’s helping real people.
Keep pushing for better. Not just more.