When you're taking medication to control seizures, planning a pregnancy shouldn't feel like choosing between two bad options. But for many women, that’s exactly what it feels like. Some of the most effective drugs for stopping seizures also carry real risks to a developing baby. The fear isn’t theoretical - it’s backed by decades of research. And yet, most people don’t know the full picture until they’re already pregnant.
Which Seizure Medications Are Riskiest During Pregnancy?
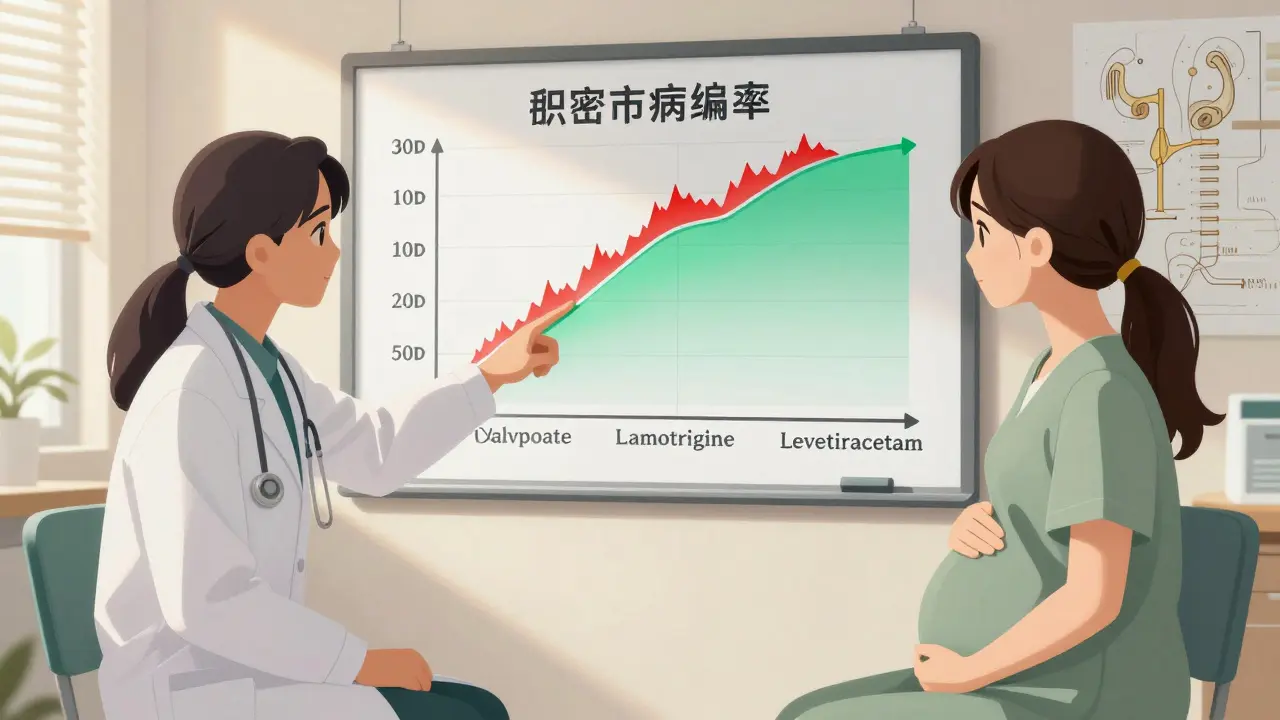
Not all seizure medications are created equal when it comes to pregnancy. The biggest red flag is valproate - also known as sodium valproate or valproic acid. It’s one of the most powerful drugs for stopping seizures, but it’s also one of the most dangerous during pregnancy. About 1 in 10 babies exposed to valproate in the womb develop major physical birth defects. That’s more than double the baseline risk seen with other seizure drugs.
These defects can include heart problems, cleft lip or palate, spine and brain malformations, and microcephaly - where the baby’s head is smaller than normal. There’s also a strong link to neurodevelopmental issues. Children exposed to valproate before birth are more than twice as likely to be diagnosed with autism spectrum disorder and nearly twice as likely to have attention deficit hyperactivity disorder (ADHD), according to a major 2020 study from Indiana University.
Other high-risk drugs include carbamazepine, phenobarbital, phenytoin, and topiramate. Each carries its own pattern of risks. For example, carbamazepine and phenobarbital are tied to higher rates of major congenital malformations when used at higher doses. Topiramate has been linked to cleft lip and low birth weight.
The good news? Not all seizure meds are risky. Two drugs - lamotrigine (Lamictal) and levetiracetam (Keppra) - have been consistently shown to be among the safest options during pregnancy. Studies tracking children exposed to these drugs in utero found no significant difference in language development, motor skills, or IQ compared to children of mothers without epilepsy. That’s a huge shift from just 20 years ago.
How Much Risk Is There, Really?
It’s easy to hear ‘birth defects’ and assume the worst. But here’s the reality: more than 90% of babies born to women with epilepsy are healthy, even when their moms take medication. The absolute risk matters more than the relative risk.
For women not taking any seizure medication, the baseline risk of a major birth defect is about 2-3%. With lamotrigine or levetiracetam, that risk stays close to that range. With valproate, it jumps to 10% or higher. That’s not a small difference - it’s a major one. And it’s why doctors now strongly advise against using valproate in women who could become pregnant, unless there’s absolutely no other option.
Even more encouraging? The overall rate of major birth defects in babies exposed to seizure meds has dropped by 39% between 1997 and 2011. Why? Because doctors are prescribing safer drugs more often. More women are getting preconception counseling. More are switching to lower-risk options before getting pregnant.
Drug Interactions: Your Birth Control Might Not Be Working
Here’s something most people don’t realize: seizure meds can mess with birth control - and birth control can mess with seizure meds. It’s a two-way street.
Drugs like carbamazepine, phenytoin, phenobarbital, and high-dose topiramate can make hormonal birth control - pills, patches, rings - much less effective. In some cases, they reduce the hormone levels so much that pregnancy can happen even if you’re taking your pill every day. That’s not a myth. It’s been documented in clinical studies.
And it works the other way too. Hormonal contraceptives can lower the blood levels of lamotrigine, valproate, zonisamide, and rufinamide. For lamotrigine, that drop can be dramatic - up to 50% in some cases. If your lamotrigine level falls too low, you could start having seizures again. That’s dangerous for you and your baby.
This isn’t just about contraception. It’s about keeping your seizures under control while avoiding unplanned pregnancy. The solution? Talk to your neurologist and gynecologist together. Consider non-hormonal options like the copper IUD, which isn’t affected by any seizure meds. Or if you’re on lamotrigine, your doctor might need to raise your dose when you start birth control - and lower it again if you stop.
Uncontrolled Seizures Are Dangerous Too
It’s tempting to think, ‘If the meds are risky, maybe I should stop them.’ But that’s one of the most dangerous myths out there.
Uncontrolled seizures - especially tonic-clonic (grand mal) seizures - can cause miscarriage, premature birth, injury to the mother, and even fetal death. A fall during a seizure can lead to trauma. Oxygen levels can drop dangerously low during prolonged seizures. The stress of frequent seizures can also harm fetal development.
As one researcher put it, there’s an ‘excruciating double bind.’ You need the meds to prevent seizures. But the meds might harm the baby. The answer isn’t to stop the meds - it’s to pick the safest one possible and use the lowest dose that still works.
Experts agree: no seizure medication is as dangerous to a pregnant woman or her baby as uncontrolled epilepsy. That’s why stopping meds without medical supervision is never recommended. The NIH, the American Epilepsy Society, and the UK’s MHRA all say the same thing: work with your doctor to switch to a safer drug before you get pregnant.
What Should You Do If You’re Planning a Pregnancy?
If you’re a woman of childbearing age and take seizure medication, here’s what you need to do - right now:
- Don’t wait until you’re pregnant. Talk to your neurologist before you even start trying. Preconception counseling isn’t optional - it’s essential.
- Get your current meds reviewed. If you’re on valproate, carbamazepine, phenobarbital, phenytoin, or high-dose topiramate, ask if switching is possible. Lamotrigine and levetiracetam are the go-to options for most women.
- Check your birth control. If you’re using hormonal methods, make sure they’re compatible with your meds. Consider switching to a copper IUD or implant if you’re on a drug that interferes with hormones.
- Take folic acid daily. At least 0.4 mg (400 mcg) before conception and through the first trimester. Some doctors recommend up to 5 mg if you’re on high-risk meds. Folic acid reduces the risk of neural tube defects.
- Monitor your drug levels. Blood tests for lamotrigine and other meds may need to be done more often during pregnancy, as your body changes how it processes them.
And if you’re already pregnant? Don’t panic. Don’t stop your meds. Call your doctor immediately. Many women switch safely during early pregnancy. Your baby’s safety depends on keeping your seizures controlled - and that’s still possible with the right plan.

Why Do Some Women Still Get High-Risk Meds?
Even with all this knowledge, some women still end up on valproate or other dangerous drugs during pregnancy. Why?
One big reason is access. A French study found that women with fewer financial resources or less education were more likely to be prescribed high-risk medications. They may not have had access to specialists. They may not have been offered alternatives. Or their doctors didn’t know the latest guidelines.
Another reason? Stubborn myths. Some doctors still believe that valproate is the only option for severe epilepsy. Or they assume a woman won’t get pregnant - even if she’s not using reliable birth control. Or they think the risks are too low to worry about.
But the data doesn’t lie. Valproate isn’t just risky - it’s avoidable in most cases. And with newer drugs like levetiracetam and lamotrigine, we now have tools that work just as well - without the same cost to the baby.
The Future Is Better Than the Past
It’s hard to believe now, but in the 1950s, women with epilepsy were often told not to marry or have children. Some U.S. states even passed laws banning marriage for people with epilepsy. That stigma shaped medical practice for decades.
Today, the story is different. We know more. We have safer drugs. We have better guidelines. We know that with the right care, most women with epilepsy can have healthy pregnancies and healthy babies.
One Stanford study tracked 298 children exposed to newer seizure meds before birth. At age two, their verbal skills were on par with children of mothers without epilepsy. That’s not a small win - it’s a game-changer.
Still, we’re not done. Eleven other seizure medications still don’t have enough data to say whether they’re safe in pregnancy. Research continues. Guidelines evolve. But the core message hasn’t changed: planning matters. Talking to your doctor before you get pregnant can make all the difference.
You don’t have to choose between controlling your seizures and having a baby. You just need the right information - and the right care team.
Can I stop my seizure medication if I’m pregnant?
No. Stopping seizure medication without medical supervision can lead to uncontrolled seizures, which are far more dangerous to both you and your baby than most medications. Always talk to your neurologist before making any changes.
Is lamotrigine safe during pregnancy?
Yes. Lamotrigine is one of the safest seizure medications for pregnancy. Studies show no significant increase in birth defects or developmental delays in children exposed to it before birth. However, its levels drop during pregnancy, so your doctor may need to adjust your dose.
Do seizure meds cause autism?
Some do - particularly valproate. Children exposed to valproate in the womb are more than twice as likely to be diagnosed with autism spectrum disorder compared to those exposed to other seizure meds. Lamotrigine and levetiracetam show no increased risk. The link is strong enough that valproate is now avoided in women who could become pregnant.
Can birth control pills interact with seizure meds?
Yes. Drugs like carbamazepine, phenytoin, phenobarbital, and high-dose topiramate can make hormonal birth control less effective. At the same time, birth control pills can lower levels of lamotrigine, valproate, and others. This can lead to unplanned pregnancy or breakthrough seizures. Talk to your doctor about alternatives like the copper IUD.
Should I take folic acid if I’m on seizure meds?
Yes. All women taking seizure meds who could become pregnant should take at least 0.4 mg (400 mcg) of folic acid daily, starting before conception. Some doctors recommend up to 5 mg daily for those on high-risk meds like valproate, as folic acid reduces the risk of neural tube defects.
Are newer seizure meds safer than older ones?
Yes. Older drugs like valproate, phenobarbital, and phenytoin carry higher risks of birth defects. Newer drugs like lamotrigine and levetiracetam have been shown to be much safer during pregnancy, with no major increase in birth defects or developmental issues. The overall rate of birth defects has dropped 39% since the 1990s because of this shift.
What if I’m already pregnant and taking valproate?
Don’t stop suddenly. Contact your neurologist right away. In many cases, switching to a safer medication like lamotrigine or levetiracetam is possible - especially in the first trimester. Your doctor will weigh the risks of continuing valproate against the risks of changing meds. The goal is to keep your seizures controlled while minimizing fetal risk.


Bridget Molokomme
February 3, 2026 AT 05:41So let me get this straight - we’re telling women to switch meds before pregnancy, but half the time their doctors don’t even know the guidelines? 😒 I had my neurologist tell me valproate was ‘fine’ until I googled it myself. Thanks, healthcare system.
Vatsal Srivastava
February 4, 2026 AT 17:29Lamotrigine is safe? Please. All this data is Western bias. In India we’ve used phenobarbital for generations and our babies are fine. Stop overmedicalizing natural biology.
Brittany Marioni
February 6, 2026 AT 00:46PLEASE, if you’re reading this and you’re on valproate - DO NOT WAIT. I was on it for years. My daughter had a cleft palate. It wasn’t ‘bad luck.’ It was preventable. I wish I’d known sooner. Talk to your doctor. Bring this article. Print it out. Bring a friend. You’re not alone. And you deserve better care. Seriously. Just. Do. It.
Monica Slypig
February 6, 2026 AT 16:36Why are we even talking about this? In America we overtest everything. In Europe they just let women have babies and deal with it. This is why our healthcare costs are insane. Just stop.
Ansley Mayson
February 7, 2026 AT 06:45Birth defect stats are inflated. Most studies don’t control for socioeconomic factors. Also, seizures kill more babies than meds. End of story.
Bob Hynes
February 8, 2026 AT 05:09As a Canadian who’s seen this play out in rural clinics - this article is a lifeline. My cousin switched from phenytoin to levetiracetam before her second kid. Her son is now 5, speaks three languages, and has zero developmental delays. It’s possible. It’s not magic. It’s just… good care.
larry keenan
February 9, 2026 AT 22:18The pharmacokinetic interactions between antiepileptic drugs and hormonal contraceptives are well-documented in the literature, particularly regarding CYP450 enzyme induction and glucuronidation pathways. Clinically, this necessitates therapeutic drug monitoring and individualized dosing regimens during preconception planning.
Nick Flake
February 11, 2026 AT 00:39Imagine if we treated every woman like she’s capable of making informed choices instead of treating her like a ticking time bomb. 🤍 You don’t need to be a scientist to understand: knowledge saves lives. And you? You’re worth the effort. Keep fighting. Keep asking. Keep switching. 💪
Akhona Myeki
February 12, 2026 AT 09:37Actually, in South Africa, we have no access to lamotrigine. It costs more than a month’s rent. So we use phenobarbital. And we are fine. This is Western privilege talking. You think everyone has a neurologist on speed dial?
Chinmoy Kumar
February 13, 2026 AT 15:01i read this and felt so much hope… my sister just switched to keppra and her seizures are way better. she’s trying for a baby now. i cried reading about the 90% healthy babies stat. thank you for writing this
clarissa sulio
February 15, 2026 AT 04:48My doctor said I could stay on topiramate. I said no. I got the copper IUD. Now I’m 8 weeks pregnant. Best decision ever.
Dan Pearson
February 15, 2026 AT 09:37Oh wow, so now we’re blaming doctors for not being perfect? Newsflash: people die from seizures too. You think your precious lamotrigine is a magic wand? Try having a tonic-clonic in the shower. Then come back and tell me what’s ‘safe’.
Eli Kiseop
February 15, 2026 AT 23:44Anyone else’s neurologist just shrug and say ‘just take folic acid’ and call it a day? Like noooooo that’s not enough