When your breathing stops repeatedly during sleep, your body doesn’t just feel tired-it’s in danger. Sleep apnea isn’t just snoring. It’s a silent threat that can lead to respiratory failure, heart problems, and even sudden death. For millions, the solution isn’t a pill or surgery. It’s a small machine that blows air into your nose while you sleep. That machine is CPAP. And when used right, it can save your life.
What Happens When You Have Sleep Apnea?
Obstructive sleep apnea (OSA) happens when the muscles in your throat relax too much during sleep. Your airway collapses, cutting off oxygen. Your brain wakes you up-just enough to gasp for air-then you fall back asleep. You don’t remember it. But your body does. Each time this happens, your blood oxygen drops. Your heart rate spikes. Your stress hormones surge. Over time, this pattern wears down your cardiovascular system. A person with severe OSA might stop breathing 30 to 40 times an hour. That’s one interruption every 90 seconds, all night long. Studies show that untreated OSA increases the risk of high blood pressure, stroke, and heart attack. It’s not just about feeling sleepy during the day. It’s about your body slowly failing from lack of oxygen.CPAP: The Gold Standard That Works-If You Use It
In 1981, a doctor in Sydney, Australia, invented CPAP. He used pressurized air to hold open the airway of a patient with severe sleep apnea. It worked. Today, CPAP is still the most effective treatment for moderate to severe OSA. It doesn’t cure it. But it stops the breathing pauses. A CPAP machine delivers steady air pressure through a mask. That pressure acts like a splint, keeping your throat open. For compliant users, it reduces breathing interruptions from 30+ per hour to fewer than 5. That’s a 90% improvement. And it’s not just about sleep quality. People who use CPAP regularly see their blood pressure drop by 2.5 to 5 mmHg. Their heart function improves. Their risk of stroke goes down. But here’s the catch: only about half of people who start CPAP keep using it after a year. Why? Masks leak. They feel claustrophobic. The air feels too dry. Some people just hate the noise. The problem isn’t the machine. It’s the setup.Oxygen Therapy Alone Doesn’t Fix Sleep Apnea
Some doctors still prescribe supplemental oxygen for sleep apnea. It sounds logical-if you’re low on oxygen, give more. But oxygen doesn’t solve the real problem: your airway is collapsing. You still stop breathing. Your brain still wakes up. Your heart still races. Oxygen might raise your blood oxygen levels a little, but it doesn’t stop the apneas. In fact, using oxygen alone can make things worse by masking the severity of the problem. Oxygen therapy has a place-but only in specific cases. For example, if someone has both OSA and severe lung disease like COPD, oxygen might be added to CPAP. But for pure obstructive sleep apnea? CPAP is the only treatment that fixes the root cause.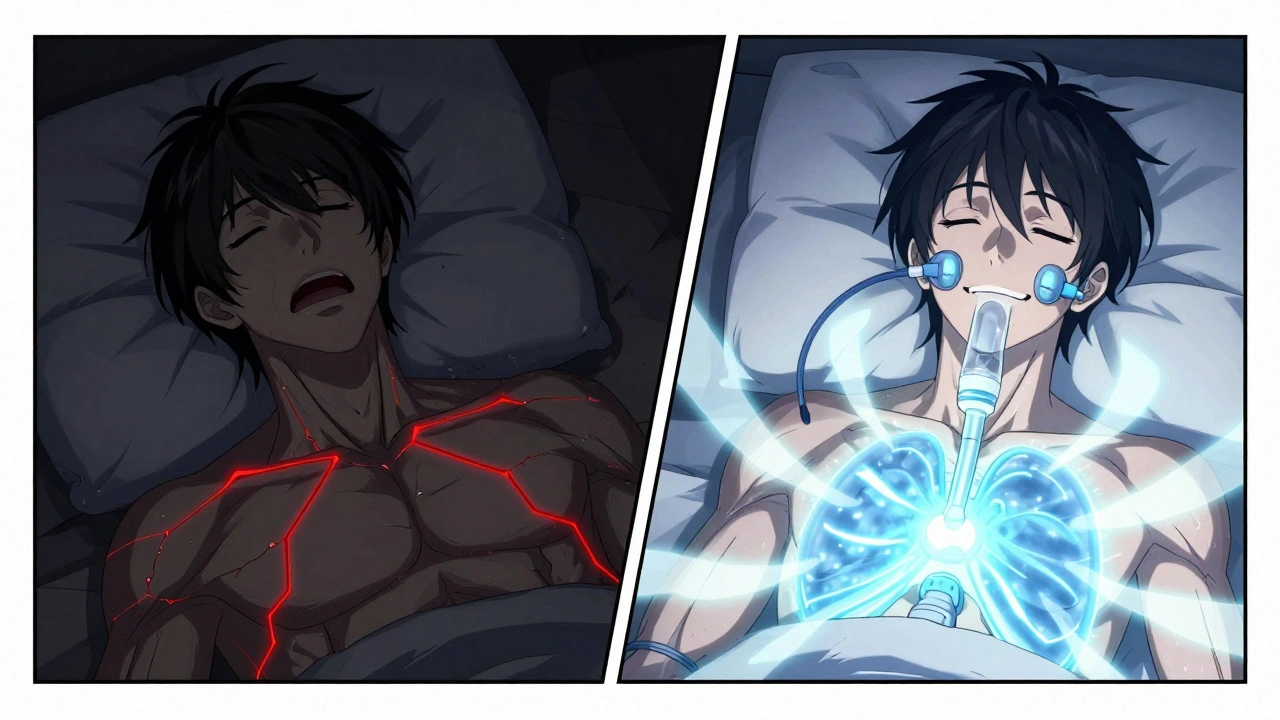
CPAP Isn’t One-Size-Fits-All
There are different types of machines. Not all CPAPs are the same.- Fixed-pressure CPAP: Delivers one set pressure all night. Good for stable cases.
- Auto-CPAP (APAP): Adjusts pressure automatically based on your breathing. Better for people whose needs change during sleep or who travel often.
- Bilevel PAP (BiPAP): Gives higher pressure when you inhale, lower when you exhale. Helps if you struggle to breathe out against the pressure.
- Adaptive Servo-Ventilation (ASV): Used for central sleep apnea, not obstructive. Not for everyone-especially not if you have heart failure.
Why People Quit CPAP-and How to Stay on Track
The biggest reason people stop using CPAP? Discomfort. A 2023 survey of over 12,500 users found that 42% quit because of mask irritation or leaks. Others say the air is too dry, or the machine is too loud. But here’s what works: structured support. People who got a 60-minute setup with a sleep technician, followed by check-ins at 72 hours and 30 days, were 32% more likely to keep using CPAP after six months. That’s not luck. That’s care. Other tips that help:- Use heated humidification. It cuts dryness and nasal irritation. 73% of happy users say it’s essential.
- Try a chin strap if you open your mouth during sleep. It stops air leaks and reduces snoring.
- Start with lower pressure and slowly increase. Don’t force yourself to use it at full strength right away.
- Use a portable CPAP for travel. Most modern devices are small enough to fit in a backpack.
What About New Alternatives?
In 2023, the FDA approved the first major alternative to CPAP: a nerve stimulator implanted in your chest. It gently wakes your tongue muscle during sleep to keep your airway open. In trials, 79% of users stuck with it after a year-much higher than CPAP’s 46%. It’s not for everyone. It’s expensive. It requires surgery. But for people who can’t tolerate CPAP, it’s a game-changer. Remote monitoring is also changing the game. New CPAP machines now send data to your doctor automatically. If your usage drops or your pressure needs change, your provider gets alerted. One platform reduced follow-up visits by 27%. No more waiting weeks for a clinic appointment.
CPAP and Respiratory Failure: The Emergency Connection
Sleep apnea doesn’t just mess with your sleep. It can trigger acute respiratory failure-especially if you have COPD or heart disease. In those cases, doctors use non-invasive ventilation (NIV), which is similar to CPAP but more powerful. NIV helps you breathe when your lungs are failing. Studies show it cuts the need for intubation by 20-30% in COPD flare-ups. The key? Timing. If NIV doesn’t improve blood oxygen and carbon dioxide levels within 1-4 hours, the risk of death rises sharply. That’s why monitoring matters. That’s why early intervention saves lives.The Bottom Line: CPAP Works. But Only If You Stick With It.
Sleep apnea is treatable. Respiratory failure from untreated apnea is preventable. CPAP is the most proven, most effective tool we have. But it’s not magic. It’s medicine. And like all medicine, it only works if you take it. If you’ve tried CPAP and quit, don’t give up. Talk to your sleep specialist. Try a different mask. Adjust the pressure. Add humidification. Use a portable unit for travel. There’s a solution that fits your life. You just have to find it.And if you’re just starting? Be patient. It takes time. But within two weeks, most users report feeling more alert, less foggy, and more alive. That’s not placebo. That’s oxygen returning to your brain-every night.
Can oxygen therapy replace CPAP for sleep apnea?
No. Oxygen therapy raises blood oxygen levels but doesn’t stop the airway from collapsing during sleep. CPAP keeps your airway open, stopping apneas at the source. Using oxygen alone may mask the severity of your condition and delay effective treatment.
How many hours per night should I use CPAP?
The standard is at least 4 hours per night on 70% of nights. But newer guidelines focus on outcomes: if your apnea-hypopnea index (AHI) stays below 5 and you feel rested, you’re doing well-even if you use it for 3.5 hours. The goal is physiological improvement, not just time on the machine.
Is CPAP covered by insurance?
Yes, in most cases. Medicare and most private insurers in the U.S. cover CPAP devices after meeting deductibles. Coverage often requires proof of usage-typically 4+ hours per night on 70% of nights. Some insurers now use remote monitoring to verify compliance.
What should I do if my CPAP mask leaks?
First, check if the mask is the right size or type. A nasal pillow may leak if you breathe through your mouth-switch to a full-face mask. Tighten straps gently; over-tightening causes more leaks. Use a chin strap if needed. Clean your mask daily-oil buildup reduces seal quality. If leaks persist, schedule a mask fitting with your sleep clinic.
Can I travel with my CPAP machine?
Yes. Most modern CPAP devices are lightweight and FAA-approved for air travel. Use a travel case and bring your power adapter. Some machines auto-adjust for altitude changes. Always carry a doctor’s note and your device’s FDA compliance label. Airlines allow CPAPs as medical devices-no extra fee.
Are there side effects of long-term CPAP use?
Most side effects are minor and fixable. Dry nose, nasal congestion, and skin irritation from masks are common but can be solved with humidification, mask adjustments, or saline sprays. Rarely, some users report bloating from swallowing air-this usually improves with pressure adjustments. Serious side effects are extremely rare.
What happens if I stop using CPAP?
Your sleep apnea returns. Within days, breathing pauses resume. Daytime fatigue, high blood pressure, and oxygen drops come back. Long-term, your risk of heart attack, stroke, and diabetes increases. Stopping CPAP isn’t a break-it’s a health setback. If you’re struggling, talk to your doctor before quitting.


Francine Phillips
December 2, 2025 AT 03:55CPAP is a nightmare. I tried it for three days and hated every second. The mask felt like a sci-fi torture device and I woke up with red marks on my face. Just sayin'.
Katherine Gianelli
December 2, 2025 AT 18:05I get it - CPAP feels like a cage at first. But after I switched to nasal pillows + heated humidifier? Game changer. I used to wake up like a zombie. Now I’m actually excited to go to bed. Don’t give up before you’ve found your fit - the right mask, the right pressure, the right support. It’s not one-size-fits-all, but it *is* life-changing if you stick with it.
Joykrishna Banerjee
December 3, 2025 AT 22:49Let’s be real - CPAP is a $1,200 Band-Aid for a problem caused by modern laziness. People sleep on their backs, eat like pigs, and then expect a machine to fix their collapsed airway. Meanwhile, in ancient India, people didn’t need CPAP - they slept on the floor, ate lentils, and didn’t have 30% body fat. This is a lifestyle failure, not a medical one. 😒
Rashmin Patel
December 5, 2025 AT 19:23Ohhh I see you, Joykrishna 😅 But let’s not throw the baby out with the bathwater - yes, lifestyle matters, but sleep apnea isn’t just about weight. I’m a yoga instructor, eat clean, and still have moderate OSA because of my jaw structure. CPAP didn’t fix my habits - it fixed my *survival*. And guess what? My husband stopped snoring so loud the neighbors called the cops. We’re both sleeping better. Oxygen therapy alone? No way. I tried it. Woke up gasping like a fish on a dock. CPAP is the only thing that kept me alive. Also - humidifier? Non-negotiable. My nose used to feel like the Sahara. Now? Smooth sailing. 🌬️💧
parth pandya
December 6, 2025 AT 19:39hey i just started cpap last week and its kinda hard but i found out my mask was too tight and i was breathing through my mouth so i got a chin strap and now its way better. also the machine is way quieter than i thought. i thought itd be a jet engine but its like a soft fan. still getting used to it but i feel less foggy already. thanks for the tips guys 😊
Albert Essel
December 7, 2025 AT 03:24There’s a critical distinction here that’s often overlooked: CPAP treats obstructive sleep apnea by maintaining airway patency; supplemental oxygen only addresses hypoxemia, not the underlying obstruction. The two are not interchangeable. Misconceptions about oxygen therapy as a standalone solution persist in clinical practice, leading to delayed diagnosis and increased morbidity. Evidence-based guidelines are clear - CPAP remains first-line for OSA. Oxygen is adjunctive, not alternative.
Charles Moore
December 7, 2025 AT 07:58Just wanted to say - if you’re struggling with CPAP, you’re not alone. I quit for two years because I felt like a robot. Then I found a sleep tech who sat with me for an hour, adjusted my mask, taught me how to breathe with it, and even sent me a little care package with extra cushions and a cool travel case. Now I use it every night. It’s not perfect. But it’s mine. And I’m alive because of it. If you’re thinking of giving up - please, reach out. Someone’s waiting to help you find your version of ‘works’.
Myson Jones
December 8, 2025 AT 17:23As someone who works in sleep medicine, I’ve seen patients go from barely functioning to vibrant, alert, and present in their families’ lives after consistent CPAP use. It’s not glamorous. It’s not quick. But it’s one of the most effective interventions in all of medicine. Don’t let the discomfort fool you - this is the quiet hero of chronic disease prevention. And yes, the data tracking? It’s not surveillance. It’s support.