Why NTI Drugs Are Different
Not all generic drugs are created equal. For most medications, swapping a brand-name pill for a cheaper generic is safe and common. But for NTI drugs - narrow therapeutic index drugs - even tiny differences in how the body absorbs the medicine can lead to serious harm. These are drugs where the line between effective and dangerous is razor-thin. A 5% change in blood levels might mean the difference between controlling seizures or triggering them. A 10% dip in warfarin concentration could cause a clot. A slight rise in lithium might lead to toxicity. That’s why states have stepped in where the federal government hasn’t.
The FDA doesn’t officially label any drug as NTI. It uses an ‘A’ or ‘B’ rating in its Orange Book to show if generics are therapeutically equivalent. But that rating allows for up to a 20% variation in absorption between brand and generic. For drugs like levothyroxine, antiepileptics, or digoxin, that 20% gap is too wide. Clinicians have seen patients stabilized for months on a brand-name version, only to have their thyroid levels go haywire after switching to a generic. Studies show over a third of patients on levothyroxine need a dose adjustment after a generic switch. That’s not a minor inconvenience - it’s a medical reset.
What States Are Doing About It
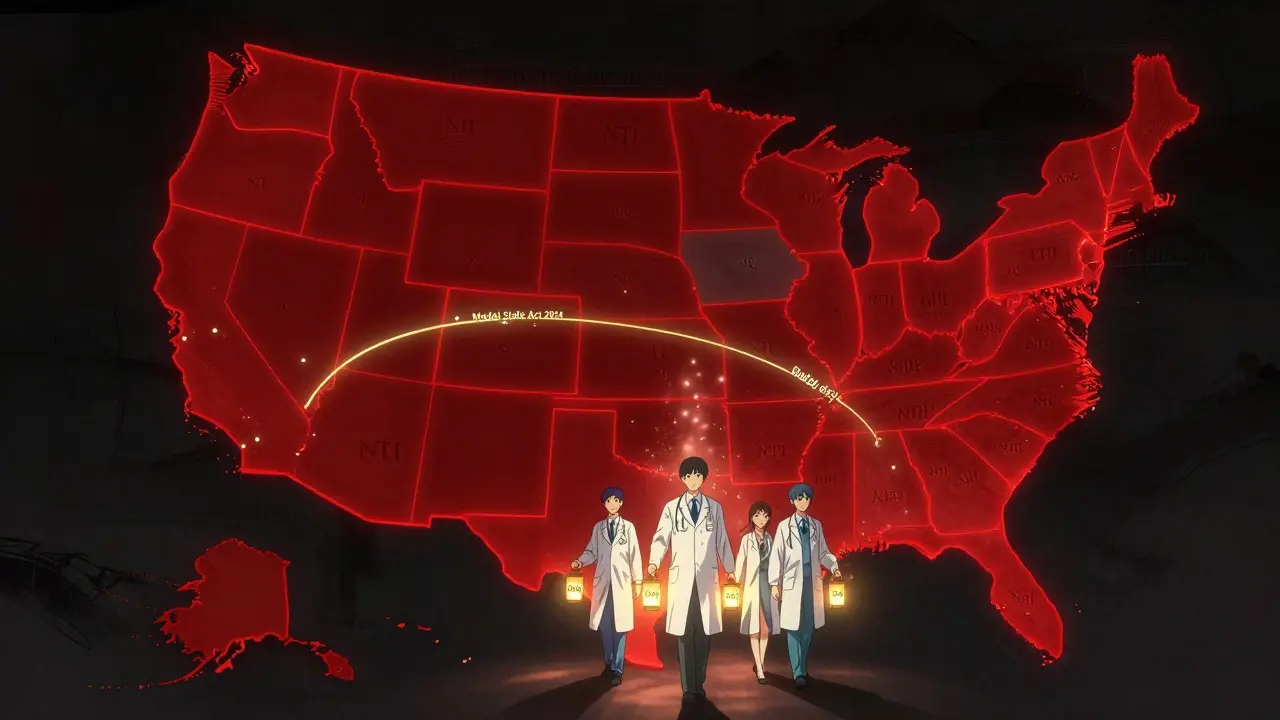
As of 2025, 27 states have laws restricting generic substitution for NTI drugs. But there’s no national standard. Each state has carved out its own rules, creating a patchwork that confuses pharmacists, prescribers, and patients alike.
In Kentucky, the Board of Pharmacy maintains a hard list of NTI drugs that cannot be substituted without a prescriber’s explicit OK. That includes warfarin, digoxin, and several antiepileptic drugs like phenytoin and carbamazepine. The law is clear: no substitution, period. Pennsylvania has a nearly identical list, with no wiggle room.
South Carolina takes a softer approach. Instead of banning substitution outright, its rules recommend against it for NTI drugs - and also for specific brand-name drugs like Synthroid and Premarin. It even includes broader categories like insulin and time-release asthma meds under its ‘critical drugs’ label. Pharmacists here aren’t breaking the law if they substitute, but they’re strongly advised not to.
Tennessee has a unique twist. It allows substitution of A-rated generics - unless the patient has epilepsy or seizures. Then, no substitution. Even if the drug isn’t on any official NTI list, the condition overrides everything. Meanwhile, Iowa tells pharmacists to rely solely on the FDA’s Orange Book and doesn’t maintain its own NTI list at all.
California’s law is among the most detailed. Under Business and Professions Code Section 4070.5, pharmacists must notify the prescriber if they substitute any drug the state defines as having a ‘narrow therapeutic range’ where a 10% or less change in blood concentration could be dangerous. That’s stricter than the FDA’s 20% standard. Texas, on the other hand, only blocks substitution for anticonvulsants when the patient has epilepsy - a narrow exception tied to diagnosis, not drug class.
Why This Patchwork Exists
The FDA’s official stance since 1997 has been that the current bioequivalence standards work for all drugs, including NTI ones. The agency argues that if a generic passes its tests, it’s safe. But that ignores real-world clinical data. Doctors and pharmacists see patients destabilized after switches. The American College of Clinical Pharmacy reviewed 17 studies and found that 32.4% of patients on brand-name levothyroxine needed a dose change after switching to generic. That’s not a fluke - it’s a pattern.
States are responding to those real outcomes. A 2022 study in the Journal of the American Pharmacists Association found states with NTI substitution restrictions saw an 18.7% drop in warfarin-related adverse events. That’s not a huge number in absolute terms - just 0.3% fewer events overall - but for the patients affected, it’s life or death. When a patient’s INR spikes after a generic switch, they could end up in the ER with a pulmonary embolism. That’s why states feel they have to act.
At the same time, the FDA’s position isn’t just bureaucratic inertia. It’s based on decades of data showing that most generic drugs perform just as well as brand-name ones. The agency argues that creating special rules for NTI drugs sets a precedent that could slow down access to affordable medications for millions. The question isn’t just safety - it’s balance.
How Pharmacists Are Managing the Chaos
Imagine you’re a pharmacist working at a chain with locations in Tennessee, Kentucky, and Missouri. In one store, you can’t substitute antiepileptics. In another, you can’t substitute anything on the NTI list. In the third, you can substitute anything with an ‘A’ rating. Now imagine you’re covering shifts across all three - and you forget which rule applies where.
A 2023 survey by the National Community Pharmacists Association found that 68.3% of pharmacists who work in multiple states have been confused about NTI substitution rules. Over 40% admitted they accidentally broke a state law in the past year. That’s not incompetence - it’s systemic failure. The rules are too complex, too inconsistent, and too poorly communicated.
Some pharmacies use software alerts to flag NTI drugs, but those alerts depend on how the drug is coded in the system. If one state calls a drug ‘critical’ and another doesn’t, the software might miss it. Pharmacists end up relying on memory, printed lists, or last-minute calls to prescribers. That’s not safe practice - it’s a stopgap.
What’s Changing in 2025
There’s momentum toward change. In January 2024, the National Association of Boards of Pharmacy released a Model State NTI Substitution Act. It proposes a single, evidence-based list of NTI drugs, adopted uniformly across states. Twelve states have already introduced legislation based on it. That’s a big deal. Right now, Kentucky’s list and Pennsylvania’s list aren’t identical. One might include a drug the other doesn’t. That creates confusion for patients who move or for pharmacies that serve cross-border populations.
The FDA, under pressure from the Senate Committee on Aging, announced in September 2024 that it’s reconsidering its stance. A Government Accountability Office report found nearly 3,000 adverse events between 2019 and 2023 that may have been linked to NTI drug substitutions. That’s not proof of causation, but it’s enough to force a reevaluation.
Meanwhile, pharmacy benefit managers are feeling the cost. Express Scripts reported that NTI substitution restrictions increased their administrative costs by 5.7% compared to standard generic swaps. That’s because every substitution requires extra steps: checking state rules, verifying prescriber notes, sometimes calling the doctor. That’s time, money, and human error waiting to happen.
What Patients Need to Know
If you take a drug like levothyroxine, warfarin, digoxin, or an antiepileptic, don’t assume your generic will be switched automatically. Always ask your pharmacist: ‘Is this the same brand I’ve been taking?’ If you’ve been stable on a brand-name version, tell your doctor you want to stay on it. Ask them to write ‘dispense as written’ or ‘no substitution’ on the prescription.
Keep a list of your NTI drugs and which version you’re on. If you switch pharmacies or move to a new state, bring that list with you. Don’t let a pharmacy’s system assume you’re fine with a switch. Your stability matters more than cost savings.
And if you notice new symptoms after a generic switch - fatigue, dizziness, irregular heartbeat, mood changes - don’t brush it off. Call your doctor. It might not be the drug, but it might be. And when it comes to NTI drugs, that ‘might’ is enough to act on.
What’s Next?
By 2027, experts predict 38 states will have adopted standardized NTI substitution rules. That’s good news for safety and consistency. But it also means fewer generic options for these critical drugs. Generic use for NTI medications could drop by over 8 percentage points compared to other drugs. That could mean higher out-of-pocket costs for patients - and more pressure on insurers to cover brand-name versions.
The real win won’t be in which drugs are restricted - it’ll be in whether the system finally aligns. A single national list, clear rules, and better communication between prescribers, pharmacists, and patients. Until then, the patchwork stays. And patients - especially those on NTI drugs - are the ones who pay the price for the confusion.


Dorine Anthony
December 17, 2025 AT 13:51Aadil Munshi
December 19, 2025 AT 08:30Elaine Douglass
December 20, 2025 AT 23:56Monte Pareek
December 22, 2025 AT 19:09James Stearns
December 24, 2025 AT 14:03Adrienne Dagg
December 25, 2025 AT 03:58Alex Curran
December 25, 2025 AT 07:55William Liu
December 27, 2025 AT 05:18William Storrs
December 27, 2025 AT 23:42