SAH Severity Calculator
SAH Severity Assessment
This tool calculates severity of subarachnoid hemorrhage using established clinical scales. Enter values to assess patient risk and expected outcomes.
Severity Assessment
Select values for both scales to see results.
Why a Guide on Subarachnoid Hemorrhage Matters
If you’re a student, resident, or anyone eyeing a role that deals with bleeding in the brain, you need a roadmap. This article pulls together the medical basics of subarachnoid hemorrhage with the steps you’ll take to study, train, and work in the field.
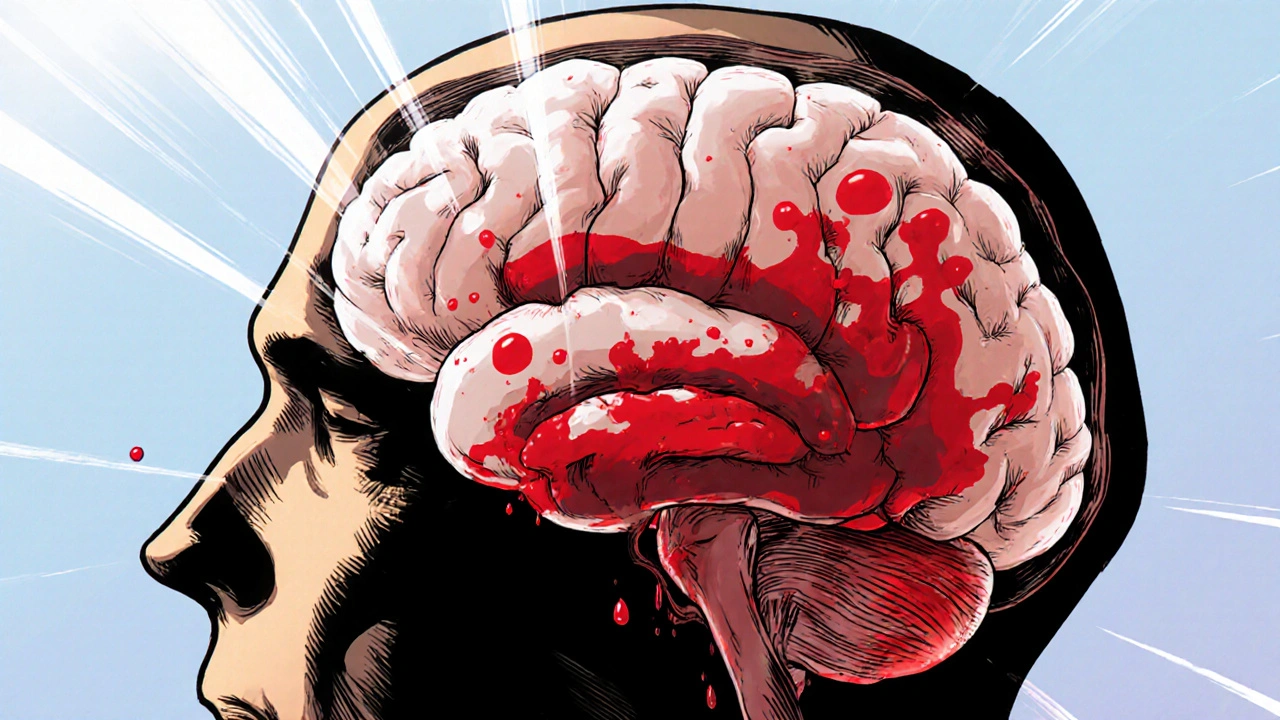
What Is Subarachnoid Hemorrhage?
Subarachnoid Hemorrhage is a type of stroke caused by bleeding into the space between the arachnoid membrane and the pia mater, the fluid‑filled “subarachnoid” compartment surrounding the brain. The most common source is a ruptured intracranial aneurysm, but arteriovenous malformations, trauma, or bleeding disorders can also be culprits. In the United States, roughly 10,000 cases occur each year, with a case‑fatality rate of about 30% before treatment.
Because the bleed pours blood directly onto the brain surface, patients can develop a sudden, thunder‑clap headache, loss of consciousness, and neurological deficits. Rapid diagnosis and specialized care are crucial for survival and functional recovery.
Key Scales: Grading the Severity
Two scoring systems help clinicians stratify risk and guide treatment decisions:
- Hunt and Hess Scale - grades I to V based on clinical presentation, from mild headache (grade I) to deep coma (grade V).
- Fisher Scale - grades the amount of blood seen on CT, ranging from none (grade 0) to diffuse thick clot (grade 4).
These scales are referenced throughout training programs and inform the urgency of interventions.
Diagnostic Toolbox
Speed matters. The typical work‑up includes:
- Non‑contrast CT scan - picks up >95% of acute bleeds within the first 6 hours.
- Lumbar puncture - performed if CT is negative but suspicion remains; xanthochromia confirms SAH.
- CT angiography (CTA) or MR angiography (MRA) - localizes the source aneurysm.
- Digital Subtraction Angiography (DSA) - gold standard for planning endovascular treatment.
Understanding when to order each study is a skill taught in both neurology and neurosurgery rotations.
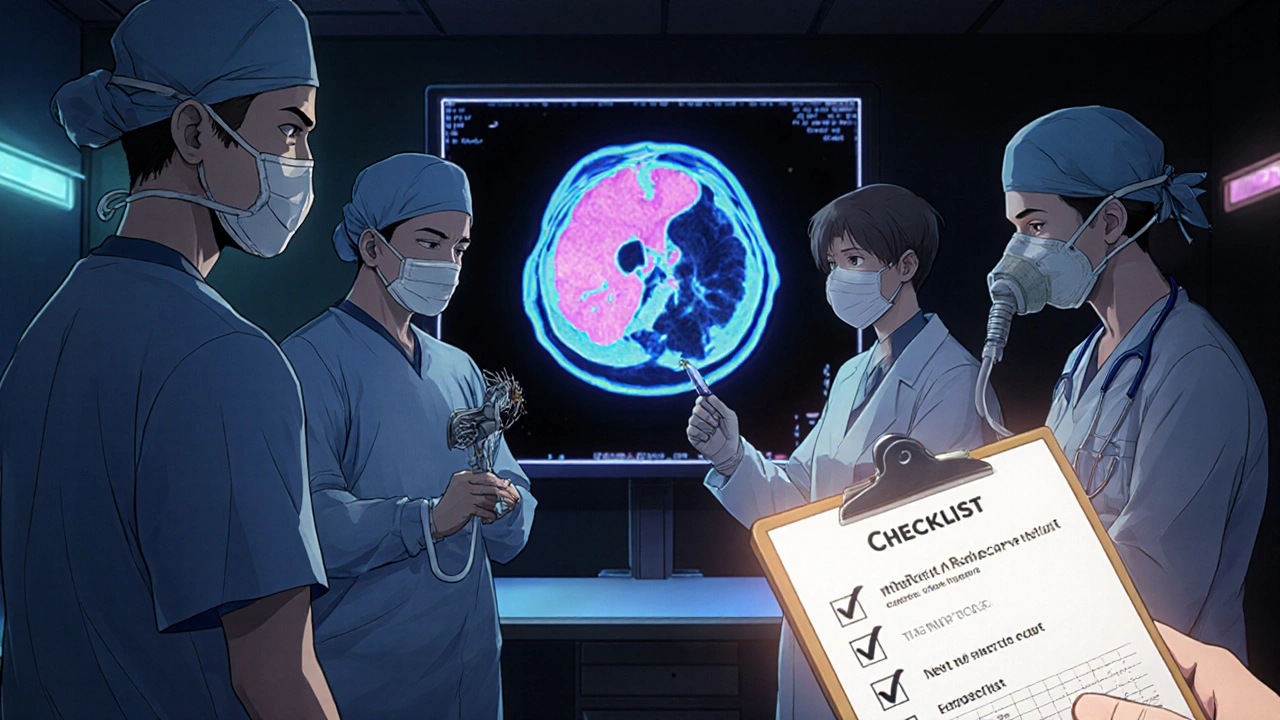
Immediate Management Overview
Once SAH is confirmed, a multidisciplinary team jumps into action. Core steps include:
- Stabilize airway, breathing, and circulation (ABCs) - most patients need intubation and blood pressure control.
- Reverse anticoagulation if the patient is on warfarin or direct oral anticoagulants.
- Administer nimodipine to reduce the risk of delayed cerebral ischemia.
- Arrange definitive aneurysm repair - either surgical clipping or endovascular coiling.
Each step falls under the purview of different specialties, which brings us to the education and career pathways.
Educational Pathway: From Classroom to Clinic
Below is a typical timeline for a U.S. medical graduate aiming to specialize in SAH care.
- Undergraduate Phase (4 years) - focus on biology, chemistry, and a strong GPA. Extracurriculars like research in neuroscience or shadowing a neurosurgeon boost your residency application.
- Medical School (4 years) - complete core rotations. The neurology and surgery clerkships are your first exposure to SAH. Take electives in cerebrovascular disease or neurocritical care if available.
- Residency (5‑7 years)
- Neurosurgery - 7 years, includes extensive exposure to clipping, endovascular basics, and ICU management.
- Neurology - 4 years, followed by a stroke fellowship (1‑2 years) where SAH cases are reviewed daily.
- Interventional Radiology - 5 years (integrated pathway) with a focus on coiling, flow diversion, and emergent endovascular techniques.
- Neurocritical Care - 1‑2 year fellowship after either neurosurgery, neurology, or anesthesiology residency.
- Fellowship (1‑2 years) - optional subspecialties: cerebrovascular surgery, endovascular neurology, or neuro‑intensive care.
Throughout training, board exams, case logs, and procedural quotas (e.g., minimum number of aneurysm clippings) are mandatory.
Career Options That Manage SAH
| Specialty | Primary Role | Typical Training Length (years) | Key Procedures | Typical Work Setting |
|---|---|---|---|---|
| Neurosurgery | Definitive aneurysm repair (clipping) and microsurgical management | 7 | Clipping, intra‑operative monitoring, external ventricular drain placement | Academic hospitals, Level‑I trauma centers |
| Neurology | Medical management, diagnosis, and long‑term follow‑up | 4 + 1‑2 (stroke fellowship) | Endovascular coiling (if dual‑trained), nimodipine administration, rehab coordination | Stroke units, outpatient clinics |
| Interventional Radiology | Endovascular occlusion of aneurysms and AVMs | 5 (integrated) or 2 (post‑residency) | Coiling, flow‑diversion, stent‑assisted techniques | Hybrid ORs, neuro‑interventional suites |
| Neurocritical Care | ICU management of SAH patients, prevention of secondary injury | 1‑2 (fellowship) | ICP monitoring, vasospasm treatment, hemodynamic optimization | Neuro‑ICU, dedicated stroke units |
Choosing a path depends on your interests: surgical precision, catheter‑based manipulation, or intensive care stewardship.
Essential Skills and Certifications
Regardless of specialty, the following credentials are often required:
- Advanced Cardiac Life Support (ACLS) - mandatory for any acute care provider.
- Neurocritical Care Board Certification - optional but highly valued for ICU roles.
- Procedural competency logs - e.g., at least 30 aneurysm clippings or 50 coilings before independent practice.
- Research methodology training - understanding of clinical trials and outcome registries such as the Hunt-Hess Registry.
Research and Academic Opportunities
SAH research is vibrant, with ongoing trials into early blood‑pressure management, novel anti‑vasospasm agents, and machine‑learning prognostic models. Getting involved early boosts your CV and opens doors to academic appointments.
Typical entry points:
- Summer research internships during medical school (often through the NIH SURE program).
- Clinical rotations on stroke teams - ask to audit outcomes or help with data collection.
- Fellowship projects - most programs require a manuscript submission before completion.
- Grant writing workshops - learn to secure funding from the American Heart Association or the NINDS.
Planning Your Career Timeline - A Checklist
- Year 1‑4 (Undergrad): Maintain GPA ≥ 3.5; seek neuroscience research.
- Year 5‑8 (Med School): Score USMLE ≥ 240; rotate in neurosurgery/neurology.
- Year 9‑15 (Residency): Log required SAH cases; obtain ACLS certification.
- Year 16‑18 (Fellowship): Publish at least one first‑author paper on SAH outcomes.
- Post‑Training: Join professional societies (AANS, CNS, American Stroke Association) and attend annual conferences.
Revisit the checklist every 2‑3 years to stay on track.
Resources for Ongoing Learning
These sites and textbooks are widely used by trainees:
- Neurosurgery by Greenberg - comprehensive chapters on aneurysm surgery.
- Stroke: Pathophysiology, Diagnosis, and Management - a go‑to reference for neurologists.
- American Heart Association Guidelines for SAH (2023 update) - downloadable PDFs.
- Neurocritical Care Society’s online webinars - recordings on vasospasm management.
Joining online forums such as the NeuroCriticalCare subreddit or the AANS mentorship network can also provide real‑world tips.
Next Steps for Aspiring SAH Professionals
Pick one concrete action today: schedule a shadowing session with a neurosurgeon, enroll in an ACLS course, or start a literature review on recent SAH trials. Small moves add up, and before you know it you’ll be part of the team that saves lives after a brain bleed.
What is the typical recovery time after a subarachnoid hemorrhage?
Recovery varies widely. Mild cases (Hunt‑Hess I‑II) may return to baseline within 3‑6 months, while severe grades (IV‑V) can require years of rehabilitation or result in permanent deficits.
Do I need a neurosurgery residency to treat SAH?
Not necessarily. Neurologists, interventional radiologists, and neuro‑intensivists also manage SAH, each focusing on different aspects of care.
How many SAH cases should I see before feeling competent?
Most boards require a minimum of 30‑50 operative or endovascular cases. Real competence often comes after 100+ supervised encounters.
What research topics are hot in SAH right now?
Early blood‑pressure targets, novel calcium‑channel blockers, machine‑learning prediction of vasospasm, and genetic risk profiling are gaining traction.
Is there a certification specifically for SAH management?
No single SAH certification exists, but neurocritical care board certification and extensive procedural logs serve as proof of expertise.

Alex Pegg
October 20, 2025 AT 19:20Reading through this guide feels like a checklist for a corporate onboarding rather than an actual medical roadmap.
Kate McKay
November 3, 2025 AT 13:32Great rundown! The step‑by‑step timeline makes the path from undergrad to fellowship feel less intimidating. I especially like the emphasis on getting research experience early – it really pays off when you’re interviewing for a neurosurgery spot. Remember to schedule that ACLS course now so you don’t have to scramble later.
Sebastian Green
November 17, 2025 AT 08:44Honestly, I’ve felt overwhelmed by the sheer number of requirements, but breaking it down like this helps. The reminder to revisit the checklist every few years is spot on; it prevents the whole process from becoming a blur.
Matthew Hall
December 1, 2025 AT 03:56Wow, who knew there were so many specialties tangled up in a single brain bleed? The neuro‑ICU crew probably earns the most coffee breaks for staying on top of vasospasm protocols.
Vijaypal Yadav
December 14, 2025 AT 23:08To add a bit more context, the Hunt‑Hess scale was originally developed in 1968 and still serves as the gold standard for initial clinical grading. Meanwhile, the Fisher scale, though simple, correlates well with the risk of vasospasm and delayed cerebral ischemia. In terms of imaging, recent advances in flat‑detector CT angiography can expedite aneurysm localization right in the angio suite, shaving off precious minutes. Also, remember that nimodipine’s benefit appears most pronounced when started within 24‑48 hours of bleed onset.
Ron Lanham
December 28, 2025 AT 18:20It is precisely the responsibility of our medical education system to ensure that aspiring practitioners are not merely trained to perform procedures but are also imbued with a profound sense of ethical duty toward patients suffering from devastating conditions like subarachnoid hemorrhage. The literature repeatedly demonstrates that mortality and morbidity are not solely functions of technical skill but are heavily influenced by how swiftly and compassionately care is delivered. Therefore, integrating communication workshops and empathy training into neurosurgical residencies is not a peripheral luxury but a core requirement. Moreover, the relentless pursuit of case numbers must never eclipse the imperative to treat each individual as a whole person, not just a collection of anatomy and imaging findings. When we discuss procedural quotas, we must also emphasize the moral obligation to mentor junior residents, ensuring they acquire competence without compromising patient safety. The same principle applies to interventional radiology fellows; they should be taught the gravity of each coil deployment, understanding that a misplaced device can spell disaster. In neurocritical care, the vigilance required to detect early signs of vasospasm is a matter of life and death, and this vigilance must be cultivated through rigorous simulation exercises. The policies set by accreditation bodies should reflect these values, mandating not only a minimum number of aneurysm clippings but also documented participation in multidisciplinary team rounds. Research, while essential, should be pursued with the ultimate goal of improving patient outcomes, not merely for the sake of academic prestige. Publishing papers without a clear translational pathway risks turning our noble profession into a vanity project. Finally, as future leaders in cerebrovascular medicine, you must advocate for public health measures that reduce the incidence of hypertension and smoking, the two biggest modifiable risk factors for SAH. Only by addressing the upstream determinants can we hope to lessen the burden of this catastrophic event. In summary, let us commit to a training paradigm that balances technical excellence with unwavering humanity, for the patients we serve deserve nothing less.
Deja Scott
January 11, 2026 AT 13:32Your call for empathy resonates deeply; compassion should indeed be woven into every training thread.
Natalie Morgan
January 25, 2026 AT 08:44Interesting piece. The checklist format really helps to visualize the path. You might add a note about the importance of mentorship in neurosurgery. Early exposure to OR cases can be a game changer.
Mahesh Upadhyay
February 8, 2026 AT 03:56All these steps are just bureaucratic fluff.
Rajesh Myadam
February 21, 2026 AT 23:08I appreciate how this guide balances hard data with practical advice. It’s comforting to see that even the most challenging SAH cases can be navigated with a clear roadmap and supportive team. Keep pushing forward.