Blood Pressure Meds: What Works, What to Watch For, and How to Stay Safe
When you’re managing blood pressure meds, prescription drugs used to lower elevated blood pressure and reduce risk of heart attack or stroke. Also known as antihypertensive drugs, they’re among the most commonly prescribed medications worldwide—and for good reason. High blood pressure often has no symptoms, but left untreated, it silently damages your heart, kidneys, and arteries. The right medicine can make a real difference, but not all blood pressure meds work the same way, and not all are safe for everyone.
There are dozens of options, each with different mechanisms. Clonidine, a drug originally developed for high blood pressure but also used for ADHD and withdrawal symptoms. Also known as alpha-2 agonist, it works by calming the nervous system to reduce heart rate and blood pressure. But it’s not always the best choice—guanfacine, a similar but longer-acting alternative often preferred for long-term use, especially in younger patients. Also known as selective alpha-2A agonist, it has fewer sedative side effects might be better. Then there are ACE inhibitors, beta-blockers, diuretics, and calcium channel blockers, each with their own pros, cons, and interactions. For example, omeprazole, a common acid-reducing drug. Also known as PPI, it can interfere with how well clopidogrel works, which matters if you’re on both for heart protection. Mixing meds without knowing these links can be dangerous.
Side effects are another big concern. Some blood pressure meds cause dizziness, fatigue, or even sexual dysfunction. Others might raise your risk of kidney issues or electrolyte imbalances. And if you’re over 65, certain drugs can increase fall risk or worsen confusion. That’s why knowing your options matters—not just which one your doctor prescribes, but why. Are you taking it because it’s cheapest? Because it’s been used for years? Or because it actually fits your body and lifestyle?
What you’ll find below isn’t just a list of articles. It’s a collection of real, practical insights from people who’ve been there. You’ll see how people compare clonidine to other options, why some switch meds after side effects, how drug interactions can sneak up on you, and what to ask your pharmacist before filling a new prescription. There’s no marketing fluff here—just straight talk about what works, what doesn’t, and how to protect yourself when you’re managing a lifelong condition.
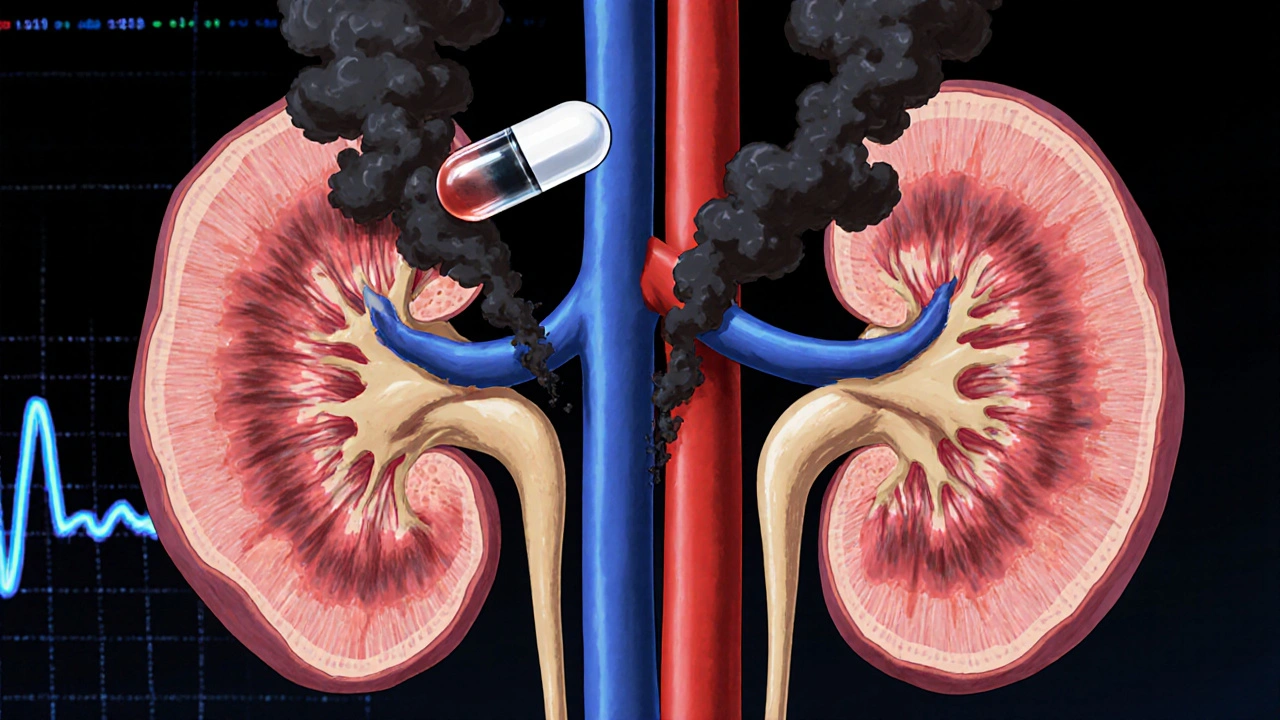
Why ACE Inhibitors Are Dangerous with Renal Artery Stenosis
Nov, 18 2025
