Medication Error Rate Calculator
How Telepharmacy Safety Compares to Traditional Pharmacies
Based on recent studies, telepharmacy medication error rates range from 0.2% to 0.8%, while traditional pharmacies range from 0.1% to 0.7%. This calculator shows how different implementation factors affect error rates.
Estimated Medication Error Rate
0.0%
This is than the national average
When you live in a rural town with no nearby pharmacy, getting your prescriptions filled isn’t just inconvenient-it can be dangerous. Missing doses, delaying refills, or skipping medications altogether because of long drives and limited hours is common. That’s where telepharmacy comes in. It’s not science fiction. It’s real. And since the pandemic, it’s been growing fast. But does it keep patients safe? What do the studies actually show?
What Telepharmacy Actually Does
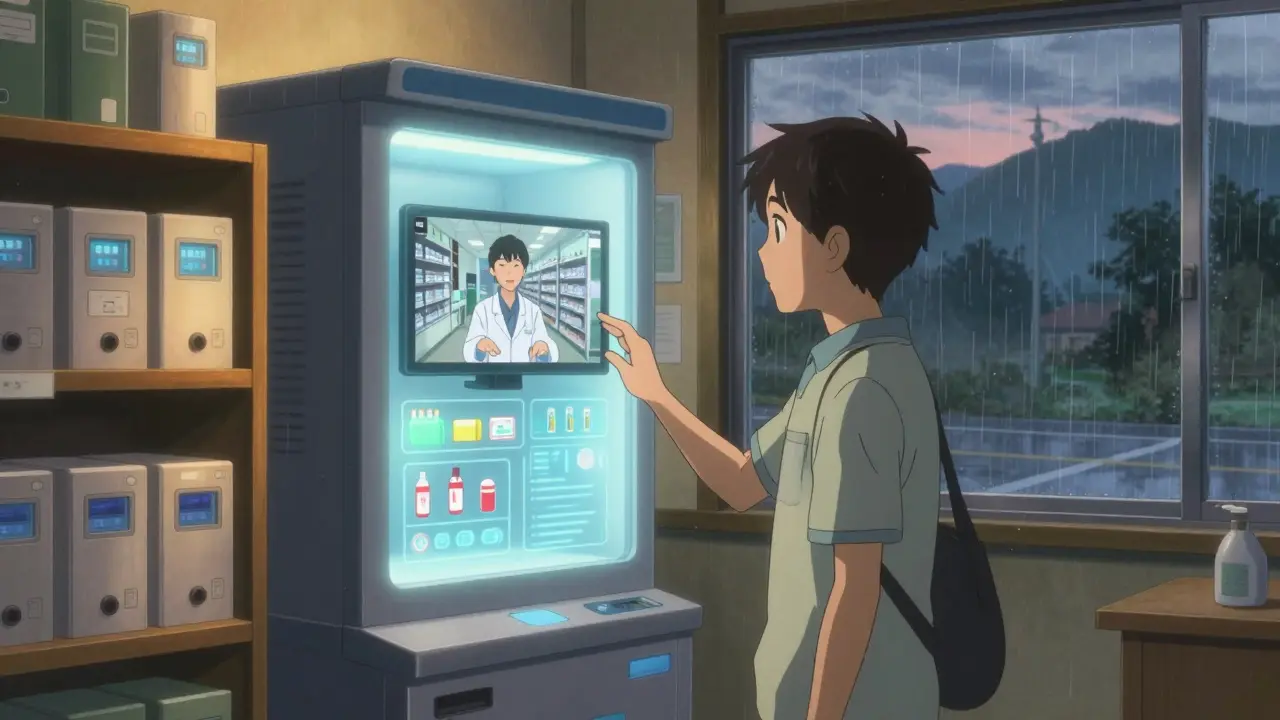
Telepharmacy isn’t just video calls with a pharmacist. It’s a full system: remote dispensing, electronic prescriptions, automated verification, and real-time consultations-all delivered through secure video platforms. Think of it like a pharmacy branch that exists online, staffed by licensed pharmacists who can review your meds, answer questions, and even fill prescriptions without you ever stepping inside a building.
The most common setup is the hub-and-spoke model. One central pharmacy, often in a city, supports multiple remote locations-like small clinics, rural hospitals, or even grocery stores in towns with no pharmacist. A technician handles the physical filling, but a pharmacist hundreds of miles away watches every step via live video. They check for drug interactions, confirm dosages, and make sure the right pill goes to the right person.
Another model is direct-to-patient. You log into a portal, chat with a pharmacist over video, and your meds get mailed to you. This works well for chronic conditions like diabetes or high blood pressure, where regular check-ins matter more than walk-in visits.
Are Telepharmacies Safe? The Numbers Don’t Lie
One of the biggest fears people have is that remote care means more mistakes. But multiple studies show the opposite. A 2021 systematic review by Pathak et al. looked at six major studies from 2010 to 2020 and found something surprising: telepharmacy medication error rates were between 0.2% and 0.8%. Traditional pharmacies? Between 0.1% and 0.7%. The difference wasn’t statistically significant. In other words, telepharmacy matches the safety of in-person pharmacies.
Even more telling: telepharmacy sites caught about 1.2 medication errors per 100 prescriptions. That’s the same rate as brick-and-mortar pharmacies. How? Remote pharmacists use automated alerts and double-check systems. They don’t get distracted by ringing phones or long lines. They focus on the script-and they catch things humans miss.
One study in JAMA Network Open (2023) showed that telepharmacy reduced after-hours drug approval times from hours down to 14-20 minutes. That’s huge for patients who need pain meds at midnight or antibiotics after hours. Faster access doesn’t just mean convenience-it prevents complications.
Where Telepharmacy Shines: Rural Areas
Here’s the real win: telepharmacy is fixing pharmacy deserts. A 2023 study found that states with strong telepharmacy laws saw a 4.5% drop in areas with zero pharmacies. In some cases, the number of people living more than 10 miles from a pharmacy fell by over 11%. That’s not a small change. It’s life-changing.
Take the Navajo Nation. Before telepharmacy, many residents drove over 50 miles for insulin or heart meds. Now, clinics on the reservation have telepharmacy kiosks. Pharmacists in Tucson review every prescription. The result? Medication error rates dropped to 0.45%, below the national average of 0.67%.
And it’s not just about access-it’s about continuity. One patient in rural Montana said video chats about her warfarin dose prevented two ER visits. That’s not luck. That’s consistent monitoring. With telepharmacy, pharmacists can track trends over time. They see when someone’s INR levels are creeping up. They adjust before it becomes an emergency.

The Hidden Risks: Tech Glitches and Missed Cues
But it’s not perfect.
Bad internet? That’s a real problem. A 2022 survey found 35% of telepharmacy sites had connection issues during consultations. One user in North Dakota had an allergic reaction because the video froze during her initial chat-and the technician didn’t catch her insulin allergy. That’s not the system’s fault. It’s a failure in protocol. If the video drops, the consultation should pause until it’s stable. Not all sites have that rule.
Then there’s the human factor. Pharmacists can’t see if a patient is sweating, trembling, or avoiding eye contact-signs that might suggest misuse or confusion. Dr. Jerry Fahrni pointed out in 2022 that non-verbal cues matter. A pharmacist in a clinic can notice a shaky hand or a confused frown. Over video? Those signs vanish.
And training gaps exist. Pharmacy students in one study performed consultations 15-20% less effectively via telepharmacy than in person. That’s not because they’re bad. It’s because they weren’t trained for it. Telepharmacy requires different skills: reading voice tone, managing tech issues on the fly, and asking the right questions without seeing the full body language.
How to Make Telepharmacy Safer
The good news? We know how to fix this.
ASHP guidelines say pharmacists need 16-24 hours of special training before doing telepharmacy work. That includes learning how to assess patients remotely, handle tech failures, and recognize red flags over video. Sites that followed this training saw 22% fewer errors.
Best practices are emerging. The Indian Health Service requires dual verification for high-risk drugs like opioids or blood thinners. If a pharmacist isn’t 100% sure, the prescription gets flagged for an in-person review. That’s smart. It doesn’t slow things down-it prevents disasters.
Also, backup systems matter. If the video cuts out, the system should auto-suspend the transaction until it’s restored. No exceptions. And identity verification? It must be foolproof. No more “Is this John Smith?” over a pixelated screen. Facial recognition or two-factor authentication should be standard.

What’s Next? AI, Regulation, and Real Data
The future of telepharmacy isn’t just better video. It’s smarter systems.
Companies like MedsAI are building AI tools that predict adverse drug events before they happen. Early trials showed an 18.7% improvement in catching dangerous interactions. Imagine a system that flags a patient’s new blood pressure med plus their existing antidepressant-and warns the pharmacist before the script is filled. That’s not coming someday. It’s here.
Regulation is catching up, too. In November 2022, Medicare started reimbursing telepharmacy services under Part D. That means more pharmacies will adopt it-and more data will be collected. The FDA’s Sentinel Initiative is now tracking telepharmacy-related adverse events in real time. And the Patient-Centered Outcomes Research Institute is funding a three-year randomized trial across 12 rural communities. That’s the gold standard. Once it’s done, we’ll finally know for sure if telepharmacy is as safe as in-person care.
The American Pharmacists Association has set a goal: establish clear safety standards for telepharmacy by 2025. That’s a big deal. Right now, 28 states have rules. 22 don’t. That patchwork creates risks. Patients shouldn’t be safer just because they live in North Dakota instead of Alabama.
Bottom Line: Safe? Yes. But Only If Done Right
Telepharmacy isn’t a magic fix. It’s a tool. And like any tool, its safety depends on how it’s used.
The evidence is clear: when implemented well, telepharmacy matches traditional pharmacies in safety. It reduces errors. It saves lives. It brings care to people who otherwise wouldn’t get it.
But poor tech, bad training, or weak protocols can undo all that. A frozen video, an untrained tech, or a rushed consultation can lead to harm.
The goal isn’t to replace in-person care. It’s to extend it-to make sure no one has to choose between their health and a 100-mile drive.
Right now, telepharmacy is at a turning point. We have the tech. We have the data. What we need now is consistency. Standardization. Accountability. If we get that right, telepharmacy won’t just be convenient. It’ll be the new normal.
Is telepharmacy as safe as a regular pharmacy?
Yes, when properly implemented. Multiple studies show telepharmacy medication error rates are comparable to traditional pharmacies-often between 0.2% and 0.8%. Remote pharmacists use automated alerts and double-check systems that can catch errors just as effectively, if not more consistently, than in-person staff. However, safety depends heavily on training, technology quality, and protocols. Poor internet, untrained staff, or rushed consultations can increase risks.
Does telepharmacy work in rural areas?
It’s one of its biggest strengths. States with strong telepharmacy laws saw a 4.5% reduction in pharmacy deserts and an 11.1% drop in the population living without nearby pharmacy access. Programs like the Indian Health Service’s telepharmacy network in Navajo Nation cut medication errors below the national average. For patients in remote areas, telepharmacy means no 50-mile drives for insulin refills or blood pressure meds-it means consistent, timely care.
What are the biggest risks of telepharmacy?
The main risks are technical failures (like poor video connections), lack of proper training for staff, and the inability to detect non-verbal cues-like tremors, confusion, or signs of misuse-that a pharmacist might notice in person. A 2022 survey found 35% of telepharmacy sites had connectivity issues. Also, some patients report feeling less confident about remote consultations. These aren’t flaws in the concept, but in how it’s executed.
Can telepharmacy detect drug interactions as well as in-person pharmacists?
Yes, often better. Remote pharmacists use software that flags potential interactions in real time, with no distractions from crowds or phone calls. Studies show telepharmacy sites catch about 1.2 errors per 100 prescriptions-matching or exceeding traditional pharmacies. The real advantage is consistency: the same pharmacist reviews every script with the same level of attention, unlike in busy retail settings where workload varies.
Is telepharmacy covered by insurance?
Increasingly, yes. Since November 2022, Medicare Part D has expanded reimbursement for telepharmacy services. Many private insurers follow suit, especially for chronic disease management. Coverage varies by state and plan, but the trend is clear: payers recognize telepharmacy reduces hospitalizations and improves adherence, making it cost-effective.
What training do telepharmacists need?
The American Society of Health-System Pharmacists (ASHP) recommends 16-24 hours of specialized training. This includes remote patient assessment, telehealth tech use, emergency protocols, and state-specific regulations. Sites with trained staff saw 22% fewer dispensing errors. Training isn’t optional-it’s essential for safety.

Emily P
December 19, 2025 AT 05:47I’ve been using telepharmacy for my dad’s blood thinners since he moved to rural Montana. The first time the video froze mid-consultation, I thought we were done for. But the system auto-paused and called us back in 90 seconds. No errors. No panic. Just tech doing its job. I didn’t know that was even a feature until now.
Jedidiah Massey
December 20, 2025 AT 19:12Let’s be clear: telepharmacy is merely a stopgap for systemic healthcare decay. The fact that we’ve normalized remote dispensing of controlled substances via pixelated screens speaks volumes about our societal collapse. The ASHP guidelines? Cute. But when your pharmacist is 300 miles away and your INR is trending up, you’re not getting care-you’re getting a compliance checklist. 😔
Alex Curran
December 22, 2025 AT 09:12Real talk: the error rates are nearly identical because the software does the heavy lifting. Humans get tired. Algorithms don’t. I’ve seen rural clinics in NSW use this model since 2019. The biggest win? Pharmacists aren’t stuck behind counters anymore. They’re doing clinical reviews. That’s a paradigm shift. Internet drops? Yeah that sucks. But fix the infrastructure not the model. 🤷♂️
Edington Renwick
December 23, 2025 AT 21:24They say it’s safe. But what about the woman in Wyoming who missed her insulin dose because the video lagged? Her husband posted about it on Reddit. It went viral. People are dying because we’re too lazy to build real pharmacies. This isn’t innovation. It’s abandonment dressed up in tech buzzwords.
Allison Pannabekcer
December 25, 2025 AT 20:18I really appreciate how this post lays out both sides. I work with elderly patients in Ohio and some of them are terrified of video calls. But once they tried it with a pharmacist who took time to explain things slowly? They cried. Not from fear-from relief. They hadn’t had a real conversation about their meds in years. It’s not perfect but it’s human. And that matters more than we admit.
Sarah McQuillan
December 27, 2025 AT 12:51Why are we even talking about this like it’s new? Europe’s been doing this since the 90s. We’re behind. And now we’re acting like it’s some revolutionary breakthrough? Also, why are we letting Medicare pay for it? Taxes shouldn’t fund tech band-aids for broken rural infrastructure. Build roads. Build pharmacies. Not apps.
Alana Koerts
December 27, 2025 AT 15:550.8% error rate? That’s still 8 errors per 1000 scripts. That’s not safe. That’s gambling. And you’re telling me we’re okay with that because it’s cheaper? No one’s talking about the downstream costs-ER visits, hospitalizations, lawsuits. This isn’t a win. It’s a liability waiting to explode.
pascal pantel
December 28, 2025 AT 18:20Let’s not sugarcoat this. Telepharmacy is a corporate cost-cutting measure disguised as healthcare equity. The real reason it’s expanding? Profit margins. Pharmacists are being replaced by remote contractors paid $25/hour. The tech? Bought from a startup that got VC funding. The patients? Afterthoughts. The data says it’s safe? That’s because they’re only measuring dispensing errors-not patient outcomes.
Chris Clark
December 29, 2025 AT 05:12Been in the Navajo Nation clinic system for 8 years. The telepharmacy kiosk? Saved my grandma’s life. She’s 82, can’t drive, no family nearby. Now she talks to the same pharmacist every week. He remembers her meds, her dog’s name, even her favorite tea. Yeah the wifi sucks sometimes. But they got backup phones. And they call if the video dies. This ain’t magic. It’s just care done right.
William Storrs
December 30, 2025 AT 00:24Look I know it sounds scary but think about it-this is how we reach people who’ve been forgotten. You don’t need a big building to save a life. You need someone who cares, even if they’re on a screen. I’ve seen patients who hadn’t filled a prescription in 18 months start taking their meds again because they finally had someone to talk to. That’s not just convenience. That’s hope.
James Stearns
December 31, 2025 AT 15:12It is my solemn duty to inform you that the current implementation of telepharmacy constitutes a material deviation from the established ethical framework of pharmaceutical practice as codified in the 1987 American Pharmaceutical Association Code of Ethics. The absence of physical presence, tactile verification, and direct sensory observation renders this modality fundamentally incompatible with the Hippocratic imperative. I urge immediate legislative review.
Nina Stacey
January 1, 2026 AT 19:50I just wanted to say thank you for writing this. My mom is in a small town in West Virginia and she used to skip her pills because the drive was too far. Now she gets her meds by mail and talks to a pharmacist every month. She says it feels like having a friend who knows her health. I cried when I heard that. It’s not perfect but it’s better than nothing. Please keep pushing for better training and better internet. We need this.