Thyroid & Immunity Symptom Checker
Select symptoms that apply to you to see how they relate to thyroid and immune health.
Your Symptom Analysis
Key Takeaways
- Thyroid hormones directly influence immune cell production and activity.
- Hypothyroidism often co‑exists with autoimmune disorders such as Hashimoto's thyroiditis.
- Low thyroid function can blunt vaccine response and increase infection risk.
- Proper nutrition, medication adherence, and stress management help keep both systems in balance.
- Regular blood tests are essential for catching problems early.
Understanding thyroid deficiency is the first step toward protecting your immune health. Below we break down what the thyroid does, how it talks to your immune system, and what you can do if the conversation goes off‑track.
What is Thyroid Deficiency?
The thyroid gland is a butterfly‑shaped organ at the base of the neck that produces the hormones triiodothyronine (T3) and thyroxine (T4). When it fails to make enough of these hormones, the condition is called hypothyroidism (commonly referred to as thyroid deficiency), leading to a slowdown of metabolism, fatigue, weight gain, and a host of other symptoms.
How the Immune System Works
The immune system is a network of cells, tissues, and organs that defends the body against infections, cancer, and other threats. Key players include white blood cells such as lymphocytes, neutrophils, and macrophages., and signaling molecules called cytokines which coordinate the immune response.. When any part of this system is out of balance, you become more vulnerable to illness.
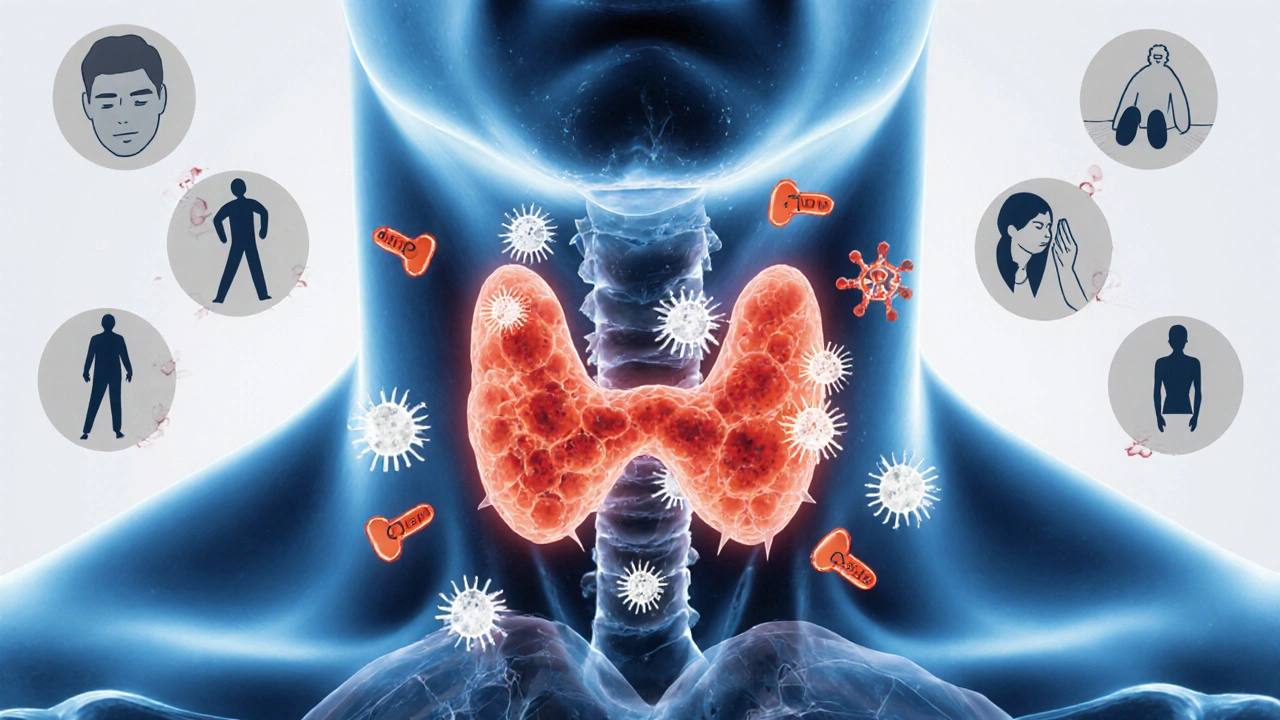
The Biological Link Between Thyroid Hormones and Immunity
Thyroid hormones act like a master switch for many cellular processes. They influence the production and maturation of white blood cells and modulate cytokine secretion. Low T3/T4 levels tend to:
- Reduce the speed at which immune cells divide, weakening the first line of defense.
- Shift the balance toward anti‑inflammatory cytokines, which can impair the ability to fight viruses and bacteria.
- Lower the expression of major histocompatibility complex (MHC) molecules, making it harder for the body to present foreign antigens to immune cells.
Conversely, an overactive immune system can damage the thyroid itself, creating a feedback loop that worsens both conditions.
Autoimmune Thyroiditis: When the Immune System Attacks the Thyroid
The most common cause of hypothyroidism in iodine‑sufficient regions is Hashimoto's thyroiditis an autoimmune disorder where antibodies mistakenly target thyroid tissue.. These antibodies-primarily anti‑thyroid peroxidase (TPO) and anti‑thyroglobulin (TG)-gradually destroy hormone‑producing cells, leading to a permanent drop in T3 and T4 levels.
Because the disease originates from the immune system, patients often experience other autoimmune conditions such as type1 diabetes, celiac disease, or rheumatoid arthritis.
Symptoms That Reveal an Immune‑Thyroid Connection
When thyroid deficiency interferes with immunity, you may notice a mix of classic hypothyroid signs and infection‑related clues:
- Persistent fatigue that doesn’t improve with rest.
- Frequent colds, sinus infections, or slow wound healing.
- Unexplained muscle aches and joint stiffness.
- Dry skin and hair loss-both signs of slowed cell turnover.
- Elevated cholesterol, a common metabolic effect that also increases cardiovascular risk.
These overlapping symptoms often lead to delayed diagnosis, especially when doctors focus on one system alone.
Managing Thyroid Deficiency to Support Immune Health
Addressing the root cause-low hormone levels-helps restore immune competence. Here’s a practical roadmap:
- Get Accurate Labs: Measure serum TSH, free T4, free T3, and thyroid antibodies. Repeat every 6-12months to track treatment.
- Take Prescribed Levothyroxine (or a T4/T3 combination) exactly as directed-usually on an empty stomach 30minutes before breakfast.
- Optimize Iodine and Selenium: Adequate iodine (150µg/day) supports hormone synthesis, while selenium (100-200µg/day) aids conversion of T4 to T3 and reduces antibody titers.
- Eat Anti‑Inflammatory Foods: Include fatty fish, berries, leafy greens, and fermented foods to nurture gut health, which in turn modulates immunity.
- Manage Stress: Chronic cortisol spikes suppress both thyroid conversion and immune function. Techniques like mindfulness, yoga, or regular walking can lower cortisol.
- Stay Active: Moderate exercise boosts circulation, improves hormone sensitivity, and enhances natural killer cell activity.
- Watch for Interactions: Calcium, iron, and certain fiber supplements can hinder levothyroxine absorption-spacing them 4hours apart is safest.
When lifestyle tweaks aren’t enough, a specialist may consider low‑dose immunomodulators or a trial of a T3‑containing medication to fine‑tune the metabolic rate.

When to Seek Professional Help
If you notice any of the following, schedule an appointment promptly:
- Rapid weight gain (>5% of body weight) over a few weeks.
- New‑onset depression or severe brain fog.
- Recurring infections that last more than 10days.
- Visible swelling in the neck (possible goitre) or a feeling of tightness.
- Elevated cholesterol (>200mg/dL) despite dietary changes.
Early intervention can halt the downward spiral between thyroid hormones and immune competence.
Quick Comparison: Hypothyroidism vs. Hyperthyroidism & Immune Impact
| Aspect | Hypothyroidism (Low T3/T4) | Hyperthyroidism (High T3/T4) |
|---|---|---|
| Metabolic Rate | Slowed - fatigue, cold intolerance | Accelerated - heat intolerance, weight loss |
| White‑Blood‑Cell Production | Reduced proliferation, slower wound healing | May cause leukocytosis but can also lead to immune over‑activation |
| Cytokine Profile | Shift toward anti‑inflammatory cytokines (IL‑10 ↑) | Pro‑inflammatory tilt (IL‑6, TNF‑α ↑) |
| Infection Susceptibility | Higher risk for viral and bacterial infections | Higher risk for autoimmune flare‑ups |
| Typical Autoimmune Links | Hashimoto's thyroiditis, celiac disease | Graves' disease, vitiligo |
Bottom Line Checklist
- Get a baseline TSH, free T4, free T3, and thyroid antibody panel.
- Take levothyroxine consistently and monitor timing with meals.
- Include iodine‑rich (seaweed, iodized salt) and selenium‑rich (Brazil nuts, fish) foods.
- Practice stress‑reduction techniques 3-4 times a week.
- Schedule follow‑up labs every 6months or sooner if symptoms change.
Frequently Asked Questions
Can low thyroid function make me get sick more often?
Yes. When T3 and T4 drop, the production of white blood cells slows and cytokine signaling becomes less efficient, which means infections can linger longer and vaccines may be less effective.
Is Hashimoto's the only autoimmune cause of hypothyroidism?
Hashimoto's is the most common, but other autoimmune conditions like lymphocytic thyroiditis or rare anti‑TSH‑receptor antibodies can also lead to low thyroid hormone levels.
Do I need to avoid soy or gluten if I have thyroid deficiency?
Soy can interfere with levothyroxine absorption, so it’s best taken several hours apart. Gluten isn’t a direct problem unless you have celiac disease, which often co‑occurs with Hashimoto's.
Can taking too much iodine worsen my thyroid problem?
Excess iodine can trigger or aggravate autoimmune thyroiditis in susceptible people. Stick to the recommended 150µg/day unless your doctor advises otherwise.
How long does it take for immune function to improve after starting thyroid medication?
Many patients notice better energy and fewer infections within 4-8weeks, but full immune normalization can take several months as hormone levels stabilize.


Stephanie Pineda
October 9, 2025 AT 21:30Reading this feels like strolling through a garden of interconnected ideas-thyroid health, immunity, nutrition-all buzzing together like springtime bees. The way you linked fatigue to immune cell division really hit home; it's like the body’s power grid is dimming one circuit at a time. I love how you didn’t just toss a list of symptoms, but actually explained the biology in plain language that even my grandma could nod along to. Also, the checklist at the end is a handy quick‑reference, kind of like a cheat‑sheet for anyone feeling lost in medical jargon. Keep sprinkling that colorful clarity-it makes the science feel alive.
Anne Snyder
October 16, 2025 AT 17:43Great synthesis of endocrinology and immunology, the integration of pathophysiology with actionable steps is commendable. The inclusion of terms like cytokine signaling pathways and hormonal feedback loops adds the necessary clinical nuance without alienating lay readers. I especially appreciate the emphasis on lifestyle interventions-nutrition, stress reduction, and sleep hygiene-as core components of a holistic management plan. Your resourceful tone encourages proactive health monitoring, aligning well with preventive medicine principles. Overall, a solid, well‑structured guide for both patients and practitioners.
Rebecca M
October 23, 2025 AT 13:57While the article is generally informative, there are several linguistic inaccuracies that merit correction; for instance, the phrase "low T3/T4 levels tend to:" should be followed by a colon, not a semicolon, and the subsequent bullet points ought to be introduced with a proper list format. Moreover, "Hashimoto's thyroiditis an autoimmune disorder" lacks a necessary comma after "thyroiditis," creating a run‑on clause. It would also improve readability to replace the ambiguous "low‑dose immunomodulators" with a more precise pharmaceutical term, such as "low‑dose methimazole" or "selective cytokine inhibitors," depending on the clinical context. Finally, the recommendation to "stay active" could be expanded to specify the intensity and duration of exercise, e.g., "moderate aerobic activity for 150 minutes per week," which aligns with established guidelines.
Bianca Fernández Rodríguez
October 30, 2025 AT 09:10i dunno why everyone is actin like this is the be all end all of thyroid stuff. sure it's cool but it ain't the only reason u get sick.
Patrick Culliton
November 6, 2025 AT 05:23Honestly, this article glosses over the real issue: most patients never get proper testing because doctors dismiss mild symptoms as "just stress." If you want a genuine solution, demand comprehensive panels and push back on the one‑size‑fits‑all prescription mindset.
Andrea Smith
November 13, 2025 AT 01:37Thank you for presenting the material with such professionalism and compassionate detail. The systematic approach to evaluation and the clear emphasis on regular laboratory monitoring are essential for optimal patient outcomes. I would also commend the inclusion of dietary sources of iodine and selenium, as such nutritional guidance empowers individuals to participate actively in their care. Please continue to share these thorough and balanced insights.
Gary O'Connor
November 19, 2025 AT 21:50Cool breakdown, mate.
Justin Stanus
November 26, 2025 AT 18:03The section on cytokine shifts really resonated with me; it explains why my recurring colds felt like they were draining more energy than usual. I've been taking my levothyroxine consistently and also adding selenium supplements as suggested, and I've noticed a subtle but definite improvement in how quickly my skin heals after minor cuts. It’s also worth noting that the article’s warning about calcium and iron interactions is something many patients overlook-spacing those meds by at least four hours can make a huge difference in absorption. Overall, the practical tips are a solid complement to the underlying science.
Claire Mahony
December 3, 2025 AT 14:17While the guide is comprehensive, it could benefit from a more balanced view on soy, as not all studies show a strong impact on levothyroxine absorption.
Andrea Jacobsen
December 10, 2025 AT 10:30I appreciate the practical checklist-it makes the whole process feel less overwhelming. Adding a reminder to discuss potential medication interactions with a pharmacist could further enhance patient safety. Also, a quick note on the importance of regular follow‑up appointments would be a nice touch for those new to managing hypothyroidism.
Andrew Irwin
December 17, 2025 AT 06:43Great points on lifestyle; I especially like the emphasis on stress management, as chronic cortisol can truly sabotage thyroid conversion. It would be helpful to include a brief mention of sleep hygiene, since inadequate rest also impairs hormone regulation.
Jen R
December 24, 2025 AT 02:57Interesting read, though I think the article could have gone deeper into the role of gut microbiota in thyroid‑immune interactions.
Joseph Kloss
December 30, 2025 AT 23:10The philosophical angle on the thyroid‑immune dialogue is thought‑provoking; it reminds us that physiological systems are not isolated machines but parts of a dynamic network. However, the article could benefit from a more critical examination of the evidence supporting selenium supplementation, as some meta‑analyses suggest limited efficacy. A balanced discussion would strengthen the overall credibility.
McKenna Baldock
January 6, 2026 AT 19:23When we contemplate the intimate liaison between thyroid hormone synthesis and immune competence, we are drawn into a discourse that transcends mere biochemical pathways and ventures into the realm of systemic harmony. The thyroid, by secreting T3 and T4, orchestrates a cascade of metabolic events that finely tune the proliferative capacity of lymphocytes, the migratory agility of neutrophils, and the cytokine milieu that governs inflammatory responses. Imagine, for a moment, the endocrine organ as a conductor, its hormonal baton setting the tempo for the immune orchestra; any discord, such as hypothyroidism, introduces a sluggish rhythm that compromises the body's defensive symphony. Moreover, the feedback loops involving hypothalamic‑pituitary‑thyroid axes are themselves subject to modulation by cytokines like IL‑6 and TNF‑α, illustrating a bidirectional conversation that can either restore equilibrium or amplify pathology. In autoimmune thyroiditis, this dialogue becomes pathological: autoreactive T‑cells and B‑cells generate anti‑TPO and anti‑TG antibodies, which in turn inflict structural damage upon the follicular epithelium, reducing hormone output and perpetuating a vicious cycle of immune activation and endocrine insufficiency.
Clinically, this interplay manifests as a constellation of overlapping symptoms-fatigue, recurrent infections, dyslipidemia-each reflecting a different facet of the disrupted network. Addressing the root cause, therefore, demands a multifaceted strategy: precise laboratory quantification of TSH, free T4, free T3, and antibody titers; judicious levothyroxine replacement calibrated to normalize TSH while considering peripheral conversion to T3; and adjunctive measures such as selenium repletion, which has been shown in some trials to attenuate antibody levels, albeit modestly. Lifestyle interventions-anti‑inflammatory diets rich in omega‑3 fatty acids, regular moderate exercise, and stress mitigation techniques-serve as ancillary supports that enhance immune surveillance and promote hormonal homeostasis. It is also prudent to monitor for drug‑nutrient interactions; calcium, iron, and certain fiber supplements can impede levothyroxine absorption, necessitating strategic timing of ingestion.
From a broader perspective, the thyroid‑immune axis exemplifies the concept of network medicine, where organ systems are viewed as interconnected nodes rather than isolated silos. Future research might explore the role of the gut microbiome as a modulatory bridge, given emerging evidence that dysbiosis can influence both thyroid autoimmunity and systemic immunity. Until such insights translate into clinical practice, the best we can offer patients is a comprehensive, evidence‑based roadmap that integrates biochemical assessment, pharmacologic precision, and holistic wellness. By honoring the complexity of this dialogue, we empower individuals to restore balance, reinforcing the notion that health is a symphony, not a solo performance.