When a woman becomes pregnant and has hypothyroidism, her body’s demand for thyroid hormone jumps almost immediately. This isn’t just a minor change-it’s a biological shift that can affect everything from her own health to her baby’s brain development. The medication she’s been taking, usually levothyroxine, may no longer be enough. Without timely adjustments, the risks are real: higher chances of miscarriage, preterm birth, and lower IQ scores in the child. The good news? With the right monitoring and dose changes, these risks drop dramatically. Studies show that properly managed thyroid levels during pregnancy can reduce miscarriage rates by up to 60% and boost a child’s IQ by 7 to 10 points compared to untreated cases.
Why Thyroid Dose Needs to Go Up
The thyroid gland produces hormones that regulate metabolism, energy, and, critically, fetal brain development. During the first trimester, the baby relies entirely on the mother’s thyroid hormone because its own gland doesn’t start working until around week 12. That means any drop in maternal hormone levels directly impacts the baby’s neurological growth. Research from the National Institutes of Health found that women with pre-existing hypothyroidism needed, on average, a 16.7% increase in levothyroxine just in the first trimester-going from 85.7 mcg per day before pregnancy to 100.0 mcg per day after conception. The American Thyroid Association (ATA) recommends increasing the dose by 20-30% as soon as pregnancy is confirmed. For some, this means taking two extra pills per week. Others may need a larger jump. If a woman was taking 75 mcg daily before pregnancy, she might need to move to 90-95 mcg right away. This isn’t guesswork-it’s based on data from over 280 pregnant women tracked in a major NIH study. The body’s need for thyroid hormone rises fast, often before a woman even knows she’s pregnant. Delaying the adjustment can be harmful.How Much to Increase: Guidelines Compared
Not all doctors agree on exactly how much to increase the dose, but they all agree that an increase is necessary. The ATA suggests 20-30% more. The American College of Obstetricians and Gynecologists (ACOG) takes a more aggressive stance, recommending an immediate 50 mcg increase for women already on levothyroxine. For women newly diagnosed with hypothyroidism during pregnancy, the starting dose depends on how high their TSH is. If TSH is above 10 mIU/L, the starting dose is 1.6 mcg per kilogram of body weight. If it’s below 10, it’s 1.0 mcg/kg. For severe cases-where TSH is over 20 mIU/L-doctors may recommend a jump of 75-100 mcg per day. Moderate cases (TSH 10-20) need 50-75 mcg increases. Even mild cases (TSH 5-10) require 25-50 mcg more. These aren’t arbitrary numbers. They’re based on clinical trials and outcomes. A 2021 study in the Journal of Clinical Endocrinology & Metabolism found that women whose doses were adjusted within four weeks of a positive pregnancy test had 23% fewer preterm births than those whose adjustments were delayed.Monitoring TSH: When and How Often
Taking more medication doesn’t help if you don’t know whether it’s working. That’s why checking TSH levels is non-negotiable. The ATA recommends measuring TSH within four weeks of any dose change and then every four weeks until levels stabilize. For women with pre-existing hypothyroidism, testing should start as early as the first prenatal visit-ideally by 6 weeks gestation. A detailed monitoring schedule from the American Academy of Family Physicians (AAFP) looks like this:- At 4-6 weeks gestation
- Every 4-6 weeks until 20 weeks
- Again at 24-28 weeks
- And finally at 32-34 weeks
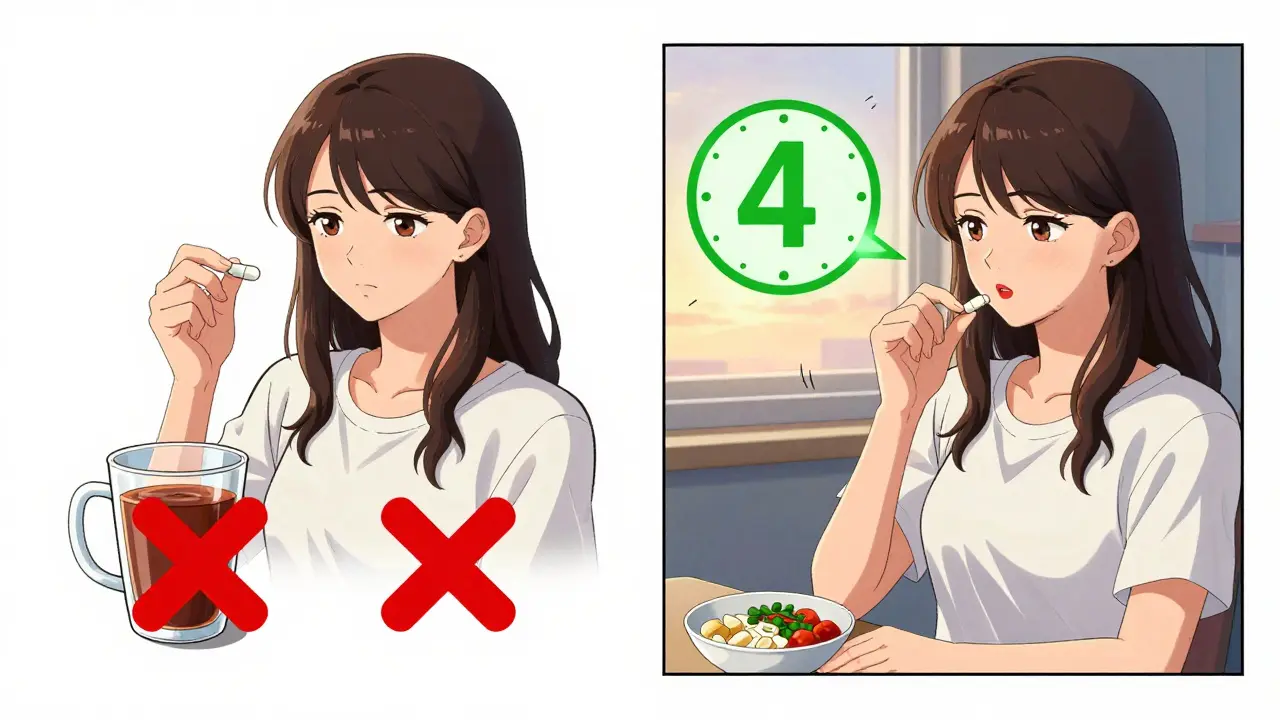
Practical Tips for Taking Levothyroxine
Taking the pill isn’t enough. How you take it matters just as much. Levothyroxine is best absorbed on an empty stomach, so it should be taken at least 30-60 minutes before eating. Many women find it easiest to take it first thing in the morning, then wait before having coffee or breakfast. Iron and calcium supplements-common during pregnancy-can cut absorption by 35-50%. That means if you’re taking prenatal vitamins with iron or extra calcium, you need to space them out. Take your thyroid pill at least four hours before or after these supplements. Some women switch to a calcium-free prenatal or take their iron at night to avoid interference. There’s also a common mistake called the “weekend effect.” Some patients increase their weekly dose by taking two extra pills on Saturday and Sunday. But this causes uneven hormone levels, with TSH spiking on Monday mornings. A better approach is to spread those extra doses across the week-maybe one extra pill on Tuesday and Thursday, for example.What Happens If You Don’t Adjust?
Ignoring dose adjustments isn’t just a technical oversight-it’s a real threat to the baby’s future. A woman with untreated or under-treated hypothyroidism during pregnancy is more likely to experience preeclampsia, placental abruption, and low birth weight. But the most concerning impact is on brain development. Studies using standardized IQ tests show that children born to mothers with high TSH in the first trimester score significantly lower than peers whose mothers had optimal levels. One patient on the EndocrineWeb forum shared her experience: “My doctor increased my dose by 50 mcg right away, but my TSH was still 4.2 at 8 weeks. I had to push for another increase. I was terrified the whole time.” Her story isn’t rare. A 2019 survey of 150 OB/GYNs found that 68% didn’t routinely check TSH at the first prenatal visit for women with known thyroid disease. That delay can cost weeks of critical brain development time.
Technology and Support Tools
Modern tools are helping close the gap between guidelines and real-world care. The “MyThyroid” app, launched in 2019, has been used by over 12,500 pregnant women. Of those, 87% reported better medication adherence and less anxiety. Electronic health records (EHRs) like Epic now include automated alerts for pregnant patients on levothyroxine, reminding doctors to check TSH and adjust doses. As of 2021, 65% of U.S. hospitals use this feature. New research is pushing things even further. The 2022 ENDO trial used artificial intelligence to predict individual dose needs based on pre-pregnancy TSH, weight, and thyroid antibodies. The AI-guided group had 28% better TSH control than those on standard dosing. The TRUST trial, expected to finish in late 2024, is testing whether personalized algorithms can make this the new standard.Global Access and Future Challenges
While technology and guidelines are improving in high-income countries, access remains a major issue elsewhere. In low-income nations, only 22% of women have consistent access to levothyroxine. This contributes to 15% of preventable developmental delays globally. The World Health Organization added levothyroxine to its Essential Medicines List for maternal health in 2023, a step toward fixing this gap. Looking ahead, experts predict thyroid management in pregnancy will become more precise. Genetic markers, AI-driven dosing, and real-time monitoring could soon be routine. But for now, the foundation remains simple: test early, adjust fast, monitor often.How soon after confirming pregnancy should I increase my levothyroxine dose?
You should increase your dose as soon as pregnancy is confirmed-ideally within days. Thyroid hormone demand rises immediately after conception, and the baby’s brain depends on your hormones during the first 10-12 weeks. Waiting until your first prenatal visit (often around 8-10 weeks) can delay critical support for fetal development. The American Thyroid Association recommends increasing your dose by 20-30% right away.
Can I take my thyroid medication with my prenatal vitamin?
No, not at the same time. Prenatal vitamins often contain iron and calcium, which can block levothyroxine absorption by 35-50%. Take your thyroid pill on an empty stomach, at least 30-60 minutes before eating. Then wait at least four hours before taking your prenatal vitamin. Many women take their thyroid pill in the morning and their prenatal at night to avoid this conflict.
What TSH level is considered safe during pregnancy?
Target TSH levels vary slightly by guideline. The American Thyroid Association recommends keeping TSH below 2.5 mIU/L throughout pregnancy. The Endocrine Society allows up to 3.0 mIU/L in the second and third trimesters. However, studies show that TSH above 2.5 in the first trimester increases miscarriage risk by 69%. Even if your doctor uses a higher target, staying below 2.5 is safest for your baby’s brain development.
Do I need to keep checking my TSH after the first trimester?
Yes. Your thyroid hormone needs keep changing throughout pregnancy. Even if your levels were perfect in the first trimester, you’ll likely need another adjustment by the second or third trimester. Most guidelines recommend checking TSH every 4-6 weeks until 20 weeks, then again at 24-28 weeks and 32-34 weeks. Hormone demand peaks near term, and your dose may need another small increase.
What if I forget to increase my dose? Can I catch up later?
It’s never too late to fix it, but the earlier you act, the better. The first trimester is the most critical window for fetal brain development. If you delayed your dose increase, get tested right away and adjust as soon as possible. Studies show that even late adjustments still improve outcomes compared to no adjustment at all. But the longer you wait, the greater the risk to your baby’s neurological development. Don’t panic-act quickly and work with your doctor to get back on track.

