Urinary Retention Risk Calculator
Calculate Your Risk
-
ACB 3
-
ACB 2
-
ACB 2
-
ACB 2
-
ACB 2
-
Imagine taking a pill for an overactive bladder, hoping to stop those sudden urges, only to find yourself unable to pee at all. It sounds rare, but it happens more often than you think - especially if you’re a man over 65 with an enlarged prostate. This isn’t a myth or a worst-case scenario from a movie. It’s a real, documented risk tied to a class of drugs called anticholinergics.
What Are Anticholinergic Drugs, Really?
Anticholinergics are medications that block a chemical in your body called acetylcholine. This chemical helps your bladder contract to push urine out. When you take an anticholinergic, you’re essentially telling your bladder to relax - which is fine if your bladder is too active. But if your bladder already struggles to empty, this can be dangerous. These drugs are commonly prescribed for overactive bladder (OAB), irritable bowel syndrome, motion sickness, and even some depression or Parkinson’s symptoms. Common names include oxybutynin, tolterodine, solifenacin, and darifenacin. Oxybutynin, one of the oldest, is still widely used - but it’s also one of the riskiest when it comes to urinary retention. The problem isn’t just the drug itself. It’s how your body responds to it. Your bladder doesn’t work like a simple on/off switch. It needs a delicate balance: the detrusor muscle (the main bladder muscle) must contract, while the sphincter (the valve at the bottom) must relax. Acetylcholine is the signal that tells the detrusor to squeeze. Anticholinergics block that signal. No squeeze = no emptying.Why Men Over 65 Are at Higher Risk
If you’re a man with benign prostatic hyperplasia (BPH) - an enlarged prostate - your urinary tract is already partially blocked. Your bladder has to work harder just to push urine past the obstruction. That means your bladder muscle is already strained. Now add an anticholinergic. It weakens the very muscle you’re relying on to get the job done. The result? You can’t fully empty your bladder. Residual urine builds up. That’s urinary retention. Studies show that in men with BPH, the risk of drug-induced retention jumps from 0.5% in the general population to 4.3%. That’s nearly nine times higher. And it’s not just theoretical. A 2022 survey of over 1,200 people taking anticholinergics found that 8.7% had to be catheterized because they couldn’t urinate. For men, the rate was 12.3%. For women, it was 5.1%. One Reddit user, 71, described his emergency room visit after taking tolterodine. Another man, 68, wrote on Drugs.com: “After two weeks of oxybutynin, I stopped peeing completely. My urologist said this happens in 1 out of 50 men my age with even mild prostate issues.” These aren’t outliers. They’re predictable outcomes.The Risk Hierarchy: Not All Anticholinergics Are Equal
Not every anticholinergic carries the same danger. The risk depends on how tightly the drug binds to the M3 receptor - the specific receptor that triggers bladder contraction. - Oxybutynin: Blocks M1, M2, and M3 receptors equally. High risk. Studies show a 2.1-fold higher chance of retention than tolterodine in men with BPH. - Tolterodine: Slightly more selective for M3. Lower risk than oxybutynin, but still dangerous in high-risk groups. - Solifenacin: 31 times more selective for M3 than M2. Moderate risk. Often preferred if anticholinergics must be used. - Darifenacin: Highly selective for M3. Lower retention risk than non-selective drugs. - Trospium chloride: Doesn’t cross the blood-brain barrier easily. Moderate to high risk, but fewer cognitive side effects. The European Association of Urology ranks oxybutynin as high risk (1.8-2.5% retention rate), solifenacin as moderate (1.2-1.8%), and trospium as moderate-high (1.5-2.2%).The Anticholinergic Burden Score: It’s Not Just One Drug
Most people don’t take just one medication. Elderly patients often take five, six, or more pills a day. Each drug adds to your total anticholinergic burden. The Anticholinergic Cognitive Burden (ACB) scale scores drugs from 1 to 3 based on how strongly they block acetylcholine. A score of 3 means high risk. A 2017 study found that people with a total ACB score of 3 or higher had a 68% increased risk of urinary retention. Think of it like this: If you’re taking oxybutynin (ACB 3), an antihistamine like diphenhydramine (ACB 3), and an antidepressant like amitriptyline (ACB 3), your total score is 9. That’s not just risky - it’s dangerous. The American Geriatrics Society’s Beers Criteria specifically lists anticholinergics as potentially inappropriate for older adults - not just because of memory problems, but because of urinary retention.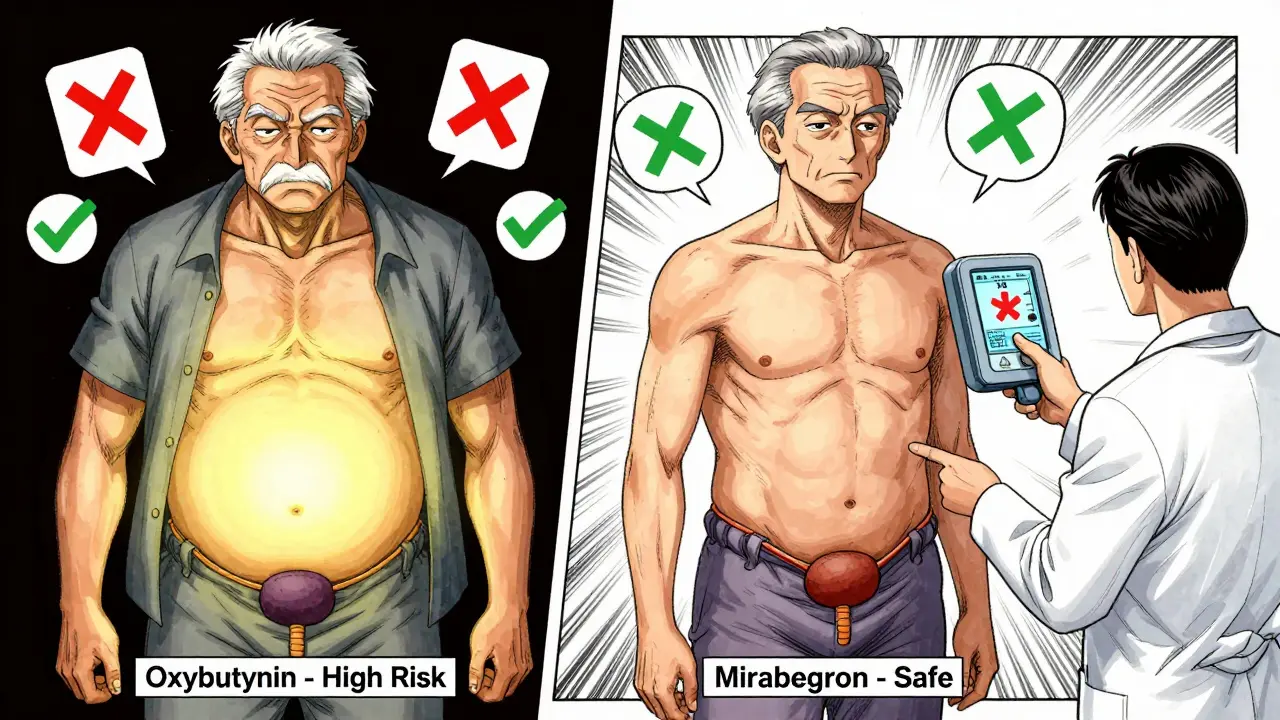
What the Experts Say
Dr. Jerry G. Blaivas, a leading urologist, says anticholinergics should be “absolutely contraindicated” in men with a history of urinary retention or significant prostate blockage. Dr. Roger Dmochowski, former president of the International Continence Society, says the risk-benefit ratio for these drugs in elderly men with prostate issues is “increasingly unfavorable.” The American Urological Association (AUA) guidelines from 2022 are blunt: don’t prescribe anticholinergics to anyone with known urinary retention. The FDA requires black box warnings on all anticholinergic labels for this exact reason. There’s some debate. Dr. Victor Nitti argues low doses can be safe with close monitoring. But Dr. Howard B. Goldman, also from AUA, says: “No level of exposure is safe in men with prior retention.” The weight of evidence leans heavily toward caution.How to Stay Safe: What You Need to Do
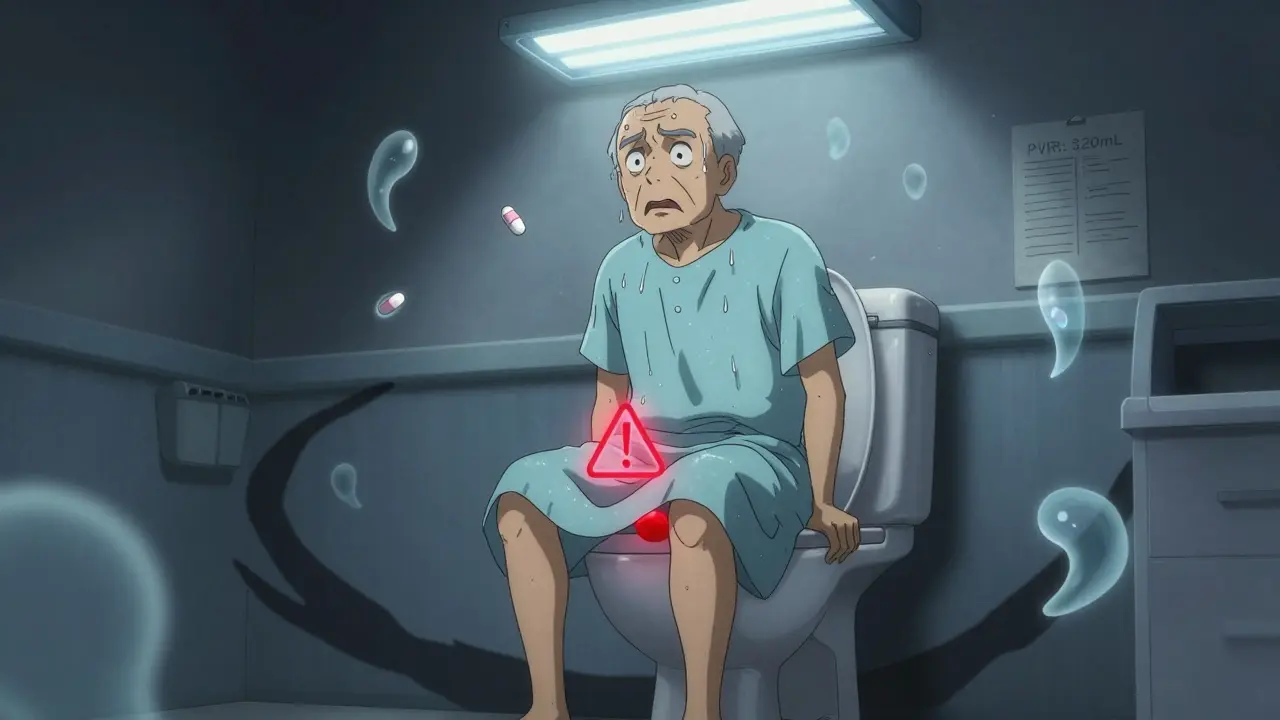
If you’re prescribed an anticholinergic, especially if you’re male, over 65, or have prostate issues, here’s what you must do:- Get a baseline post-void residual (PVR) test before starting the drug. This measures how much urine is left in your bladder after you pee. Normal is under 50mL. If it’s over 100mL, you’re already at risk.
- Monitor PVR regularly. The AUA recommends checking it weekly for the first month, then quarterly. Many clinics use a handheld bladder scanner - it’s quick, painless, and non-invasive.
- Know the warning signs. Straining to start urinating, weak stream, feeling like you haven’t emptied, or needing to go again right after - these are red flags.
- Call your doctor if you can’t pee for 12 hours. Acute urinary retention is a medical emergency. You’ll need a catheter.
- Ask about alternatives. Mirabegron (Betmiga) works differently - it relaxes the bladder muscle by stimulating beta-3 receptors. Retention risk? Just 0.3%. That’s less than a third of anticholinergics.
What Are the Alternatives?
You don’t have to live with an overactive bladder - or risk retention. - Mirabegron: First-line for men. No anticholinergic effect. Lower retention risk. May cause high blood pressure, so monitor if you’re hypertensive. - OnabotulinumtoxinA (Botox): Injected directly into the bladder. Reduces urgency and frequency. Retention risk is only 0.5%, but you may need to self-catheterize temporarily. - Peripheral neuromodulation: A small device stimulates nerves to improve bladder control. No drugs. No retention risk. Works well for stubborn cases. - Behavioral therapy: Bladder training, timed voiding, pelvic floor exercises. Often overlooked, but effective - especially when combined with other treatments. Market trends reflect this shift. In 2015, anticholinergics made up 58% of OAB prescriptions. By 2022, that dropped to 36%. Mirabegron now holds 31% of the market. Doctors are moving away from anticholinergics - especially for men.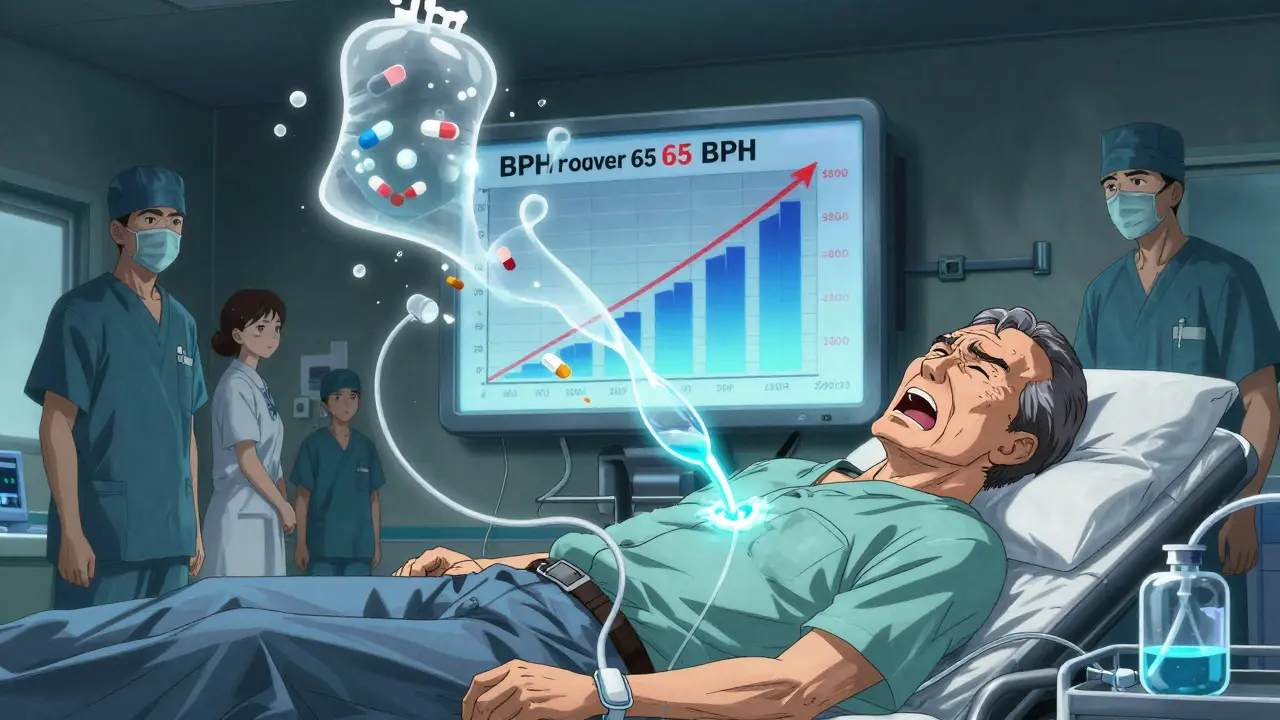
Real-World Consequences
The cost isn’t just physical. Anticholinergic-induced urinary retention costs the U.S. healthcare system $417 million a year in ER visits, catheterizations, and hospital stays. Medicare and Medicaid now penalize hospitals for “hospital-acquired” urinary retention linked to these drugs. That means hospitals are being forced to rethink prescriptions. In Europe, the EMA now requires all anticholinergic labels to say: “Contraindicated in patients with urinary retention.” That’s not a suggestion. It’s a legal warning.What’s Next?
New tools are emerging. A 2023 risk calculator called ARC uses age, prostate size, baseline PVR, and other meds to predict your personal risk with 89% accuracy. Genetic testing for CHRM3 receptor variants is also in early research - some people are genetically wired to be more sensitive to anticholinergics. The AUA’s 2025 draft guidelines may soon say: “Avoid anticholinergics entirely in men with prostate volume over 30mL.” That’s not far-fetched. It’s based on real data.Bottom Line
Anticholinergics aren’t evil drugs. They help millions. But they’re not safe for everyone. If you’re a man over 65 with prostate issues, or if you’re already having trouble emptying your bladder, these drugs can turn a manageable condition into a medical emergency. Don’t assume your doctor knows your full picture. Bring up the risk. Ask for a PVR test. Ask about mirabegron. Ask if you really need this drug at all. Your bladder doesn’t have a backup plan. Once it stops working, you’re left with a catheter - and a lesson learned too late.Can anticholinergic drugs cause urinary retention in women?
Yes, but less often than in men. Women have a 5.1% risk of retention from anticholinergics, compared to 12.3% in men. This is because women don’t typically have prostate enlargement, which is a major contributing factor. However, women with pelvic organ prolapse, nerve damage, or prior pelvic surgery are still at increased risk. The same monitoring rules apply: check post-void residual before and during treatment.
Is urinary retention from medications permanent?
Usually not - if caught early. Stopping the drug often restores normal bladder function within days to weeks. But if retention goes untreated for too long, the bladder muscle can stretch and weaken permanently. This can lead to chronic urinary retention, where you always feel like you haven’t emptied - even after stopping the medication. That’s why early detection and PVR monitoring are critical.
What should I do if I can’t urinate after starting a new medication?
If you haven’t been able to urinate for 12 hours or more, go to the emergency room immediately. Acute urinary retention is a medical emergency. You’ll need a catheter to drain your bladder. Do not wait. Do not try to force it. Do not rely on home remedies. This is not something you can treat yourself. Call your doctor after you’re stabilized, but don’t delay care.
Are there any over-the-counter meds that can cause urinary retention?
Yes. Many OTC drugs have anticholinergic effects. These include sleep aids like diphenhydramine (Benadryl, Tylenol PM), cold medicines like chlorpheniramine, and some stomach remedies like hyoscyamine. Even some allergy pills can contribute. If you’re taking multiple OTC meds, your total anticholinergic burden might be higher than you realize. Always check the active ingredients and talk to your pharmacist or doctor if you’re unsure.
Can I switch from an anticholinergic to mirabegron safely?
Yes, and it’s often recommended - especially for men with prostate issues. Mirabegron works differently: it relaxes the bladder muscle by activating beta-3 receptors, not by blocking acetylcholine. Studies show it has a much lower risk of retention (0.3% vs. 1.7% for anticholinergics). Your doctor will likely taper you off the old drug slowly and start mirabegron at a low dose. Blood pressure should be monitored, as mirabegron can raise it slightly in some people.

Matt Beck
January 5, 2026 AT 13:39Molly McLane
January 6, 2026 AT 08:10Katie Schoen
January 6, 2026 AT 10:58Cam Jane
January 8, 2026 AT 00:36Wesley Pereira
January 8, 2026 AT 02:28Amy Le
January 9, 2026 AT 10:48Pavan Vora
January 10, 2026 AT 04:39Stuart Shield
January 11, 2026 AT 06:54Susan Arlene
January 13, 2026 AT 05:42Mukesh Pareek
January 13, 2026 AT 07:28Ashley S
January 13, 2026 AT 22:50Jeane Hendrix
January 14, 2026 AT 20:48Rachel Wermager
January 16, 2026 AT 16:41Katelyn Slack
January 18, 2026 AT 13:15