ACE Inhibitors: How They Lower Blood Pressure and What Alternatives Work
When your doctor says you need an ACE inhibitor, a class of drugs that block the enzyme responsible for narrowing blood vessels, helping reduce blood pressure. Also known as angiotensin-converting enzyme inhibitors, they're one of the most prescribed treatments for hypertension, heart failure, and kidney protection in diabetics. But they’re not magic pills—some people get a dry cough, others can’t tolerate them at all. And if you’re on other meds like clonidine, a blood pressure and ADHD medication that works differently by calming nerve signals, switching or combining them needs care. That’s why understanding how ACE inhibitors fit into your overall treatment plan matters more than just taking the pill.
These drugs work by stopping your body from making angiotensin II, a chemical that tightens blood vessels. Less tightening means lower pressure, less strain on your heart, and better blood flow to your kidneys. But here’s the catch: they don’t work the same for everyone. Studies show Black patients often respond better to other classes like calcium channel blockers. And if you have kidney disease, your doctor might still choose an ACE inhibitor—but only if your creatinine levels are stable. You also need to watch out for drug interactions, when two or more medications interfere with each other’s effects. For example, mixing ACE inhibitors with NSAIDs like ibuprofen can hurt your kidneys. Even some supplements like potassium salts can become dangerous when combined. That’s why reading your prescription label and talking to your pharmacist isn’t optional—it’s essential.
Many people switch from ACE inhibitors because of side effects, not because they don’t work. That’s where alternatives like angiotensin receptor blockers (ARBs), a similar class of drugs that block the same pathway without causing the cough come in. Or maybe you’re looking at beta-blockers, medications that slow your heart rate and reduce blood pressure by blocking adrenaline. Or perhaps you’ve heard about calcium channel blockers, drugs that relax blood vessels by limiting calcium flow into heart and artery cells. Each has pros and cons. Some are cheaper. Some work better for older adults. Some have fewer side effects. The right one depends on your age, other conditions, and what your body tolerates.
What you’ll find below aren’t just generic drug lists. These are real stories and practical guides from people who’ve been there—how they managed side effects, why they switched from lisinopril to losartan, how they caught a dangerous interaction with potassium supplements, and what alternatives actually worked when ACE inhibitors didn’t. You’ll see how patient experiences, not just clinical trials, shape real-world choices. Whether you’re just starting treatment or tired of the cough and frustrated with your current meds, the posts here give you the unfiltered details you won’t get from a pamphlet.

Diabetic Nephropathy: How ACE Inhibitors, ARBs, and Protein Control Protect Your Kidneys
Dec, 23 2025
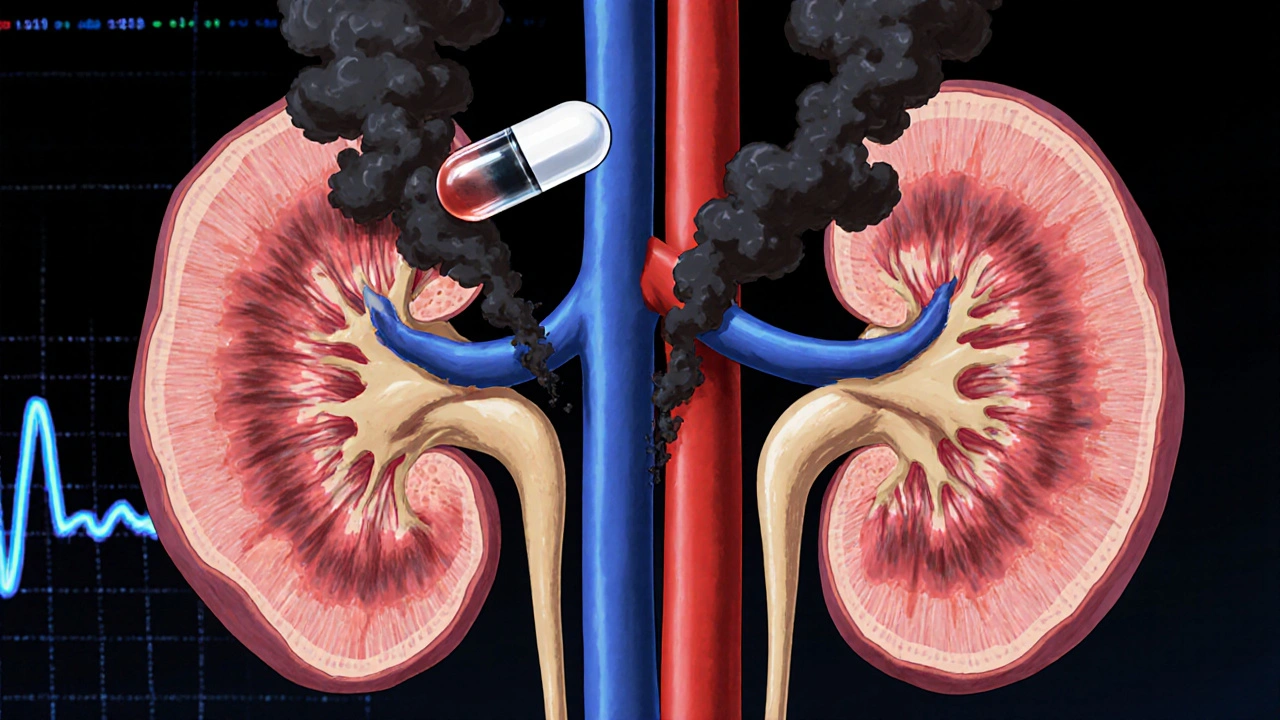
Why ACE Inhibitors Are Dangerous with Renal Artery Stenosis
Nov, 18 2025
