Clopidogrel Effectiveness: How Well It Works and What Affects It
When your doctor prescribes clopidogrel, a prescription antiplatelet drug used to prevent blood clots in people with heart disease or after a stroke. Also known as Plavix, it's one of the most common drugs given after a heart attack or stent placement to keep your arteries open. But how well does it actually work? It’s not magic—it works by blocking platelets from sticking together, which stops clots from forming in your blood vessels. For many people, it cuts the risk of another heart attack or stroke by about 20% over a year. But that number isn’t the same for everyone. Some people’s bodies don’t process clopidogrel well, making it less effective—and that’s something you need to know.
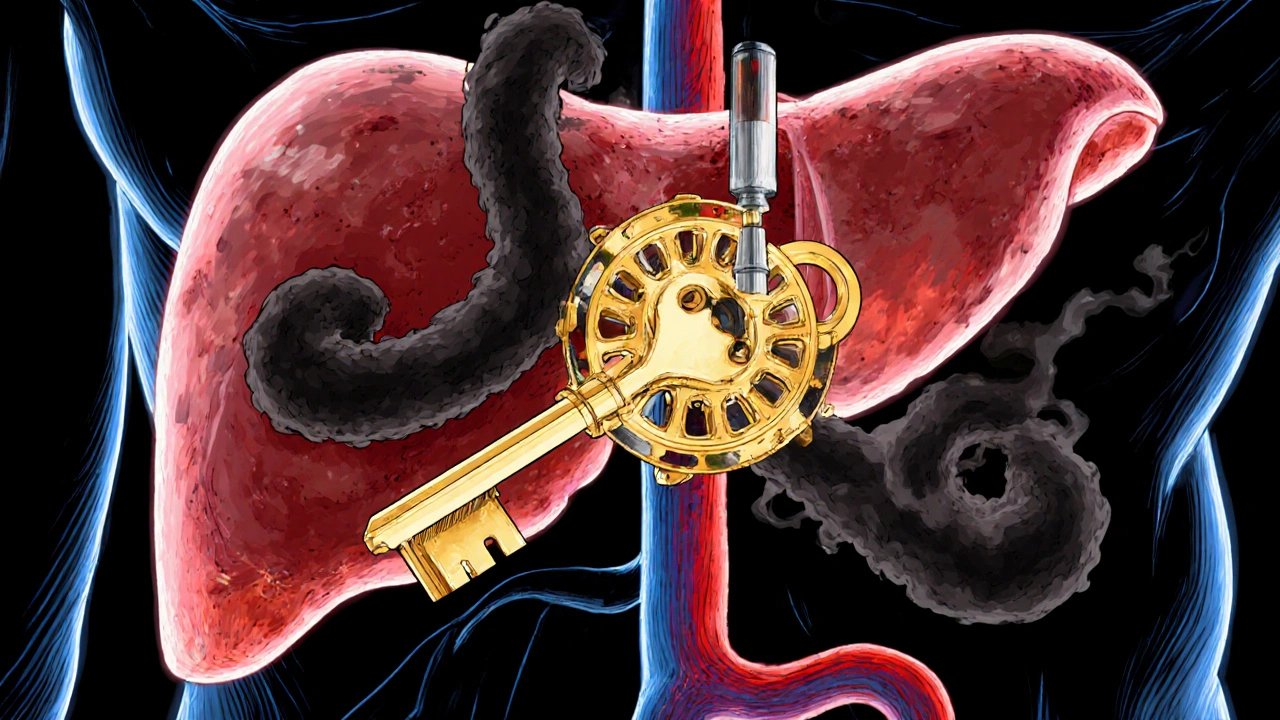
One big reason clopidogrel might not work as expected is genetics. About 30% of people carry a gene variant (CYP2C19 loss-of-function) that makes their liver unable to convert clopidogrel into its active form. If you’re one of them, you’re getting a pill that’s basically inert. That’s why some doctors test for this before prescribing it, especially if you’ve had a stent or a recent clot. Another factor is what else you’re taking. Common stomach meds like omeprazole can interfere with clopidogrel’s action, so if you’re on both, talk to your pharmacist. And then there’s compliance—missing doses or stopping early because you feel fine is one of the biggest reasons clopidogrel fails. It’s not a drug you take until you feel better. It’s a drug you take because your body needs it to stay protected.
Some people wonder if clopidogrel is better than aspirin. For most people with a history of heart disease, combining both for a short time after a stent gives better protection than either alone. But long-term, clopidogrel alone often beats aspirin in preventing repeat events, especially in high-risk patients. Still, it’s not without risks. Bleeding is the main concern—bruising easily, nosebleeds, or even internal bleeding. That’s why it’s never a casual choice. It’s prescribed when the benefit clearly outweighs the risk. And if you’ve had a bad reaction to clopidogrel, alternatives like ticagrelor or prasugrel exist. They work faster and stronger, but they’re pricier and carry higher bleeding risks too.
What you’ll find in the posts below are real-world stories and facts about how clopidogrel fits into daily life—what affects its performance, how patients manage side effects, what happens when it doesn’t work, and how it compares to other blood thinners. You’ll see how drug interactions, patient behavior, and even diet play a role. No theory. No fluff. Just what people actually experience when they take this drug long-term, and what doctors recommend when things go off track.
Omeprazole and Clopidogrel: How CYP2C19 Inhibition Affects Heart Drug Effectiveness
Nov, 2 2025
