Ischemia: Causes, Risks, and How Medications Help Manage It
When your body doesn’t get enough blood, ischemia, a condition where tissue doesn’t receive sufficient oxygen-rich blood. Also known as tissue hypoxia, it’s not a disease on its own—it’s a warning sign something’s wrong with your circulation. This can happen in your heart (called heart ischemia, reduced blood flow to the heart muscle, often due to blocked arteries), your brain (cerebral ischemia, a drop in blood flow to the brain that can lead to stroke), or even your legs, kidneys, or intestines. It’s not rare. Millions live with it, often without knowing, until symptoms like chest pain, numbness, or sudden confusion hit.
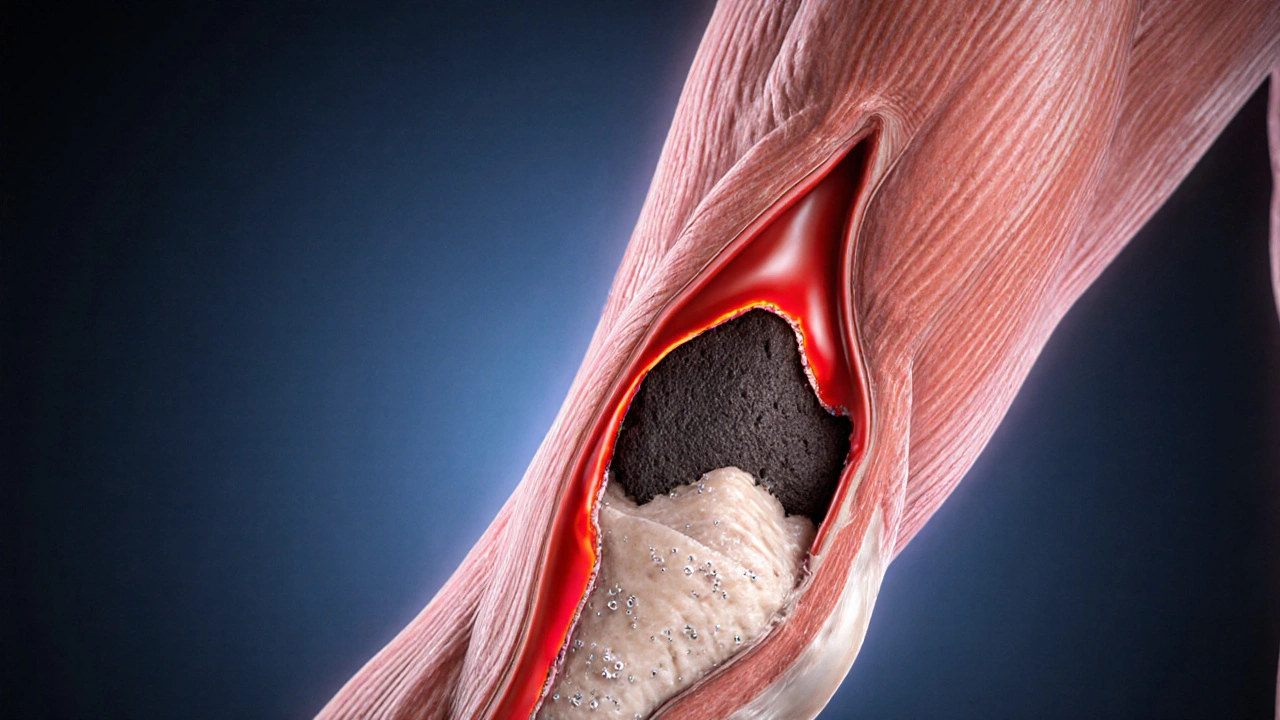
Ischemia doesn’t come out of nowhere. It’s usually tied to blood flow, the movement of oxygenated blood through arteries and capillaries being slowed or blocked. Plaque buildup from high cholesterol, blood clots, artery spasms, or even low blood pressure can trigger it. If your heart’s arteries narrow, you get angina. If a clot cuts off blood to your brain, it’s a stroke. The longer ischemia lasts, the more damage it causes—sometimes permanent. That’s why managing it isn’t just about feeling better now. It’s about preventing heart attacks, strokes, and organ failure down the road. Medications like aspirin, statins, beta-blockers, and anticoagulants don’t cure ischemia, but they help keep blood moving, reduce clots, and lower the pressure that squeezes your arteries shut.
You’ll find real-world advice here on how these drugs work, what side effects to watch for, and how they fit into daily life. Whether you’re managing heart ischemia after a diagnosis, helping a loved one with cerebral ischemia, or just trying to understand why your doctor prescribed a new pill, this collection gives you clear, no-fluff info. You’ll see how people actually cope—with medication schedules, lifestyle changes, and knowing when to call a doctor. No theory. No jargon. Just what works.
Genetics and Ischemia: How Your DNA Affects Risk
Oct, 11 2025
