Neurosurgery Career: What It Takes, What It Involves, and How It Connects to Medication Safety
When you think about a neurosurgery career, a highly specialized medical field focused on surgical treatment of the brain, spine, and nervous system. Also known as brain surgery, it requires years of intense training, steady hands, and an unshakable focus on patient outcomes. This isn’t just about cutting into the skull—it’s about understanding how every drug, from sedatives to anticonvulsants, affects the brain during and after surgery.
A neurosurgery career, a highly specialized medical field focused on surgical treatment of the brain, spine, and nervous system. Also known as brain surgery, it requires years of intense training, steady hands, and an unshakable focus on patient outcomes. This isn’t just about cutting into the skull—it’s about understanding how every drug, from sedatives to anticonvulsants, affects the brain during and after surgery.
Neurosurgeons don’t work in a vacuum. They rely on precise drug interactions, real-time monitoring of neurological responses, and careful management of side effects. Think about how medication safety, the practice of ensuring drugs are used correctly to avoid harm, especially in high-risk procedures becomes life-or-death when a patient is under anesthesia for a tumor removal. A single misread label, a missed interaction, or an unmonitored mood swing from steroids like prednisone can derail recovery. That’s why neurosurgeons pay close attention to how drugs like clozapine alter sleep architecture, how levofloxacin affects nerve function, or how dopamine agonists like ropinirole interact with post-op brain chemistry.
You’ll also find that neurosurgery overlaps with conditions covered in many of the posts here—like how neurology, the medical specialty focused on diagnosing and treating disorders of the nervous system ties into panic disorder’s effect on memory, or how hyperprolactinaemia can slow thinking after brain surgery. Even something as specific as pediatric glaucoma eye drops connects: if a child’s brain development is affected by pressure, neurosurgeons may be called in. These aren’t random topics—they’re pieces of the same puzzle.
There’s no room for guesswork in this field. That’s why neurosurgeons read drug labels like a pilot reads flight instruments. Boxed warnings, pharmacy stickers, contraindications—they’re not just fine print. They’re the difference between a successful operation and a catastrophic mistake. And when patients go home after surgery, the job doesn’t end. Managing long-term side effects of drugs like bicalutamide or diclofenac, understanding how genetics influence drug response through pharmacogenetics, or knowing when to switch from one antipsychotic to another—all of this becomes part of the neurosurgery workflow.
What you’ll find in the posts below isn’t just a list of drug guides. It’s a map of the real-world medication landscape neurosurgeons navigate every day. From how local anesthesia works in the mouth to how air pollution can worsen neurological outcomes, these articles give you the practical, no-fluff insights that matter when lives are on the line. Whether you’re considering this career, supporting someone in it, or just trying to understand why brain surgery demands such strict drug control, these posts connect the dots.
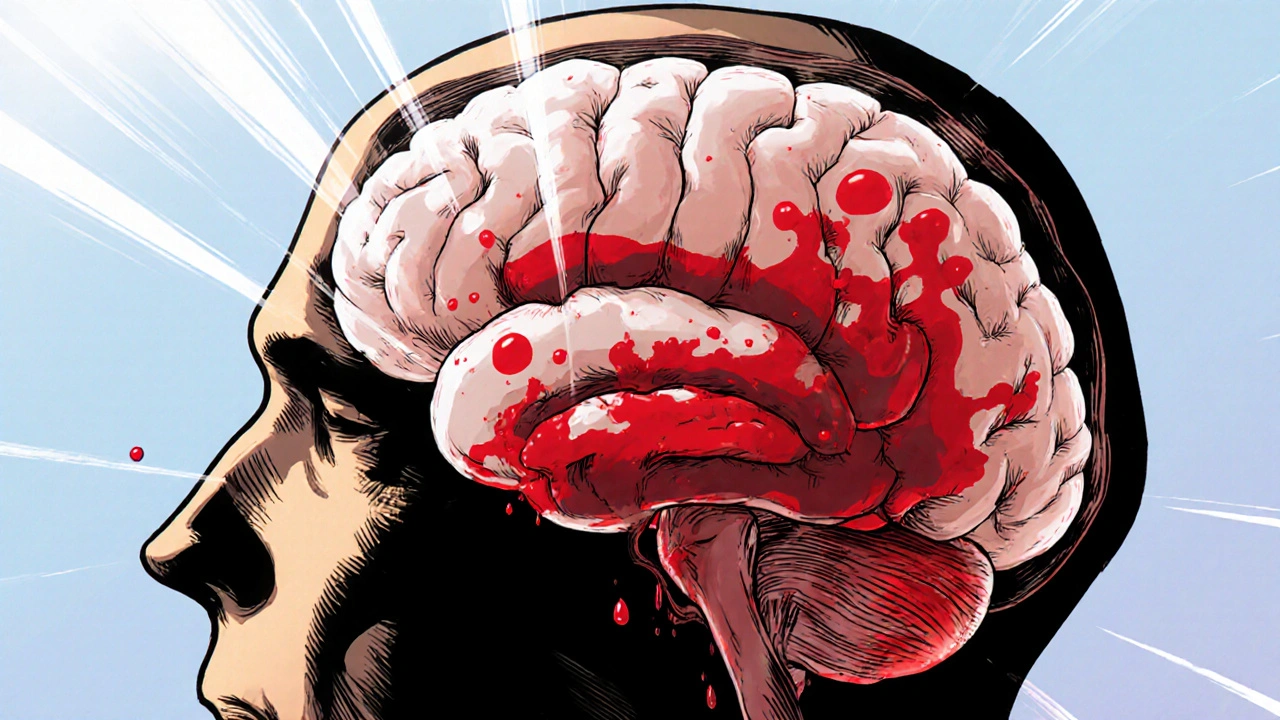
Subarachnoid Hemorrhage: Education, Training, and Career Paths Explained
Oct, 20 2025
