PPI and Antiplatelet Drugs: What You Need to Know About Interactions and Risks
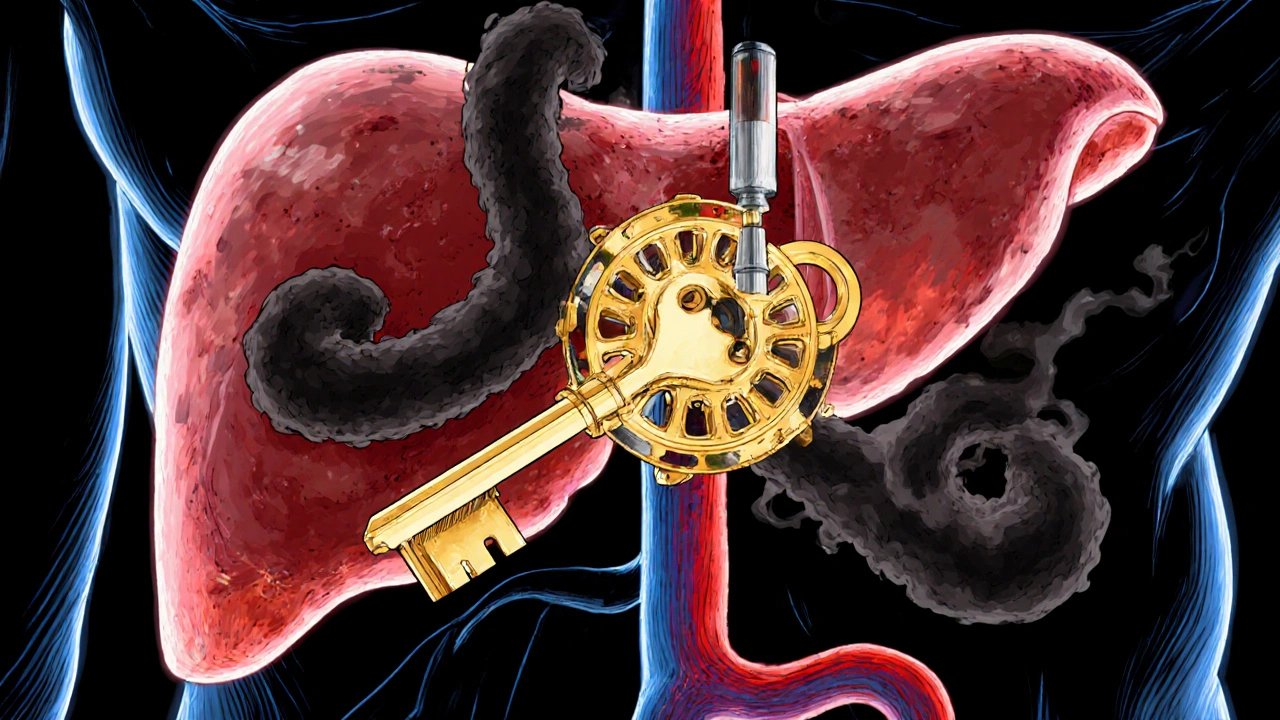
When you take a proton pump inhibitor, a class of drugs used to reduce stomach acid, often prescribed for heartburn, ulcers, or GERD. Also known as PPI, it works by blocking the acid-producing pumps in your stomach lining. Many people also take antiplatelet drugs, medications like clopidogrel or aspirin that prevent blood clots by stopping platelets from sticking together. Also known as blood thinners, they’re critical after heart attacks, stents, or strokes. The problem? These two types of drugs don’t always play nice together.
Here’s the real issue: some PPIs, especially omeprazole and esomeprazole, can block the enzyme your body needs to activate clopidogrel. That means clopidogrel doesn’t work as well — and your risk of another heart attack or stroke goes up. This isn’t theory. Studies from the FDA and major medical journals show this interaction can cut clopidogrel’s effectiveness by up to 50%. Not everyone needs to avoid PPIs — but if you’re on clopidogrel after a stent, you need to know which PPIs are safer. Pantoprazole and dexlansoprazole are less likely to interfere. And if you’re on aspirin instead of clopidogrel, the risk is much lower.
It’s not just about heart drugs. People on both PPIs and antiplatelets often have other conditions — high blood pressure, diabetes, kidney disease — and those add layers of complexity. You might be taking five or six meds, and not all your doctors are talking to each other. That’s why reading your prescription labels matters. Look for boxed warnings. Ask your pharmacist: "Does this PPI interfere with my blood thinner?" Don’t assume it’s safe because it’s over-the-counter. Even a short course of omeprazole from the pharmacy can mess with your heart medication.
If you’ve been told you need a PPI long-term, ask about alternatives. H2 blockers like famotidine can reduce acid without the same interaction risk. Lifestyle changes — smaller meals, no late-night eating, quitting smoking — can help too. And if you’re on clopidogrel, don’t stop it without talking to your doctor. The risk of clotting is real. But you also don’t want to be on a PPI that’s making your antiplatelet drug useless.
This page collects real stories and practical guides from people managing these drugs. You’ll find posts on how to read your medication labels, what to ask your pharmacist, which PPIs are safest with clopidogrel, and how to spot hidden risks in your regimen. Whether you’re a senior on multiple meds, a post-stent patient, or just trying to understand why your doctor switched your acid medicine, you’ll find clear, no-fluff advice here.
Omeprazole and Clopidogrel: How CYP2C19 Inhibition Affects Heart Drug Effectiveness
Nov, 2 2025
