Drug Interactions: What You Need to Know
Ever taken a pill and felt weird afterward? Chances are you’ve experienced a drug interaction, even if it didn’t feel dramatic. An interaction happens when two or more substances—prescriptions, over‑the‑counter meds, supplements, or even food—affect each other’s effectiveness or cause side effects. Understanding the basics can stop a minor inconvenience from turning into a health scare.
First, know that not every mix is dangerous. Some combos are harmless, and a few even boost each other's benefits. The trick is to spot the risky ones before they cause trouble. That means paying attention to what you’re taking, reading labels, and asking the right questions.
Common Interaction Mistakes to Watch Out For
Many people assume a prescription is the only thing they need to track, but supplements and diet can be just as powerful. St. John’s Wort, for example, can lower the levels of birth‑control pills, making them less effective. Similarly, calcium‑rich foods can interfere with antibiotics like doxycycline, reducing absorption and leaving the infection untreated.
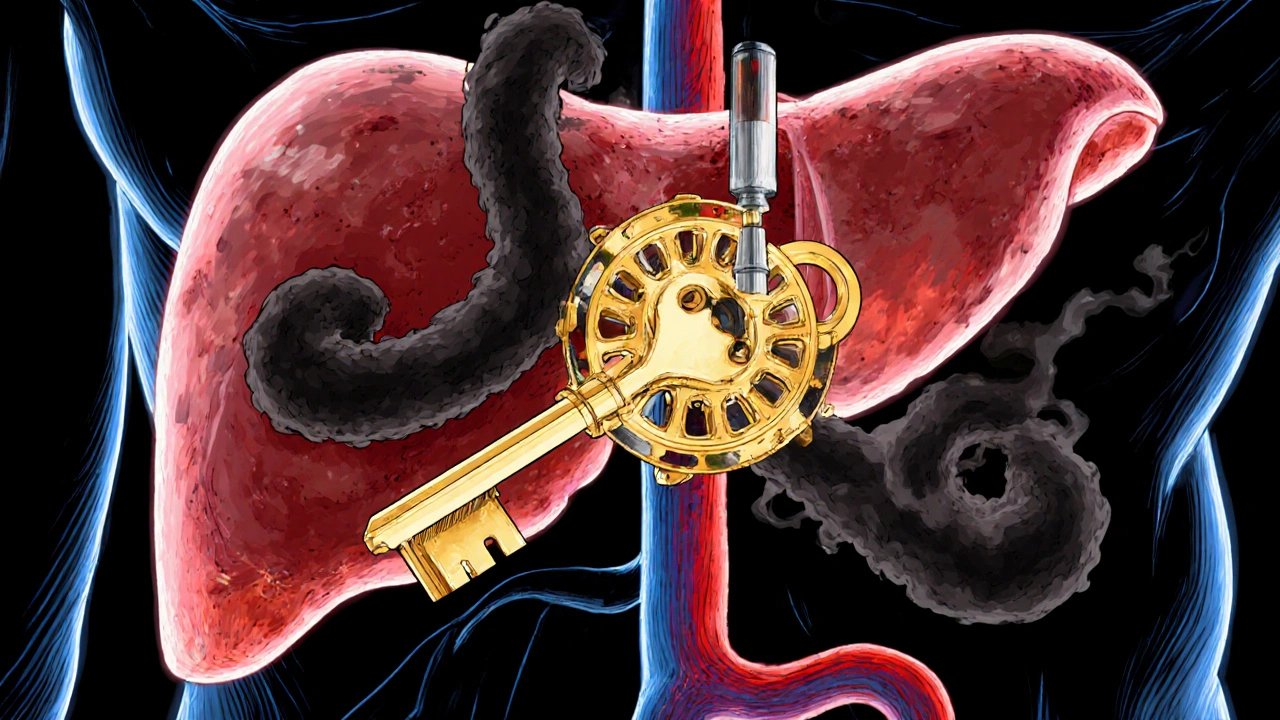
Another frequent slip is mixing pain relievers. Taking ibuprofen with a blood thinner such as warfarin can increase bleeding risk. Even over‑the‑counter cold medicine can raise blood pressure if you’re already on a hypertensive drug. If you’re juggling several prescriptions—say, a heart medication, a cholesterol pill, and a mood stabilizer—double‑check that none share a metabolic pathway that could cause a buildup.
Finally, timing matters. Some drugs need a gap of a few hours from food or other meds. Levaquin (levofloxacin) should be taken on an empty stomach, while calcium supplements should be spaced away from it. Missing these windows can lower the drug’s impact and make you think the treatment isn’t working.
Tools & Steps to Keep Your Meds Safe
Start by creating a master list of everything you take—prescriptions, vitamins, herbal teas, even the occasional energy drink. Write down the dosage, frequency, and why you’re using it. Keep this list on your fridge or in a note‑taking app so you can pull it up quickly at the pharmacy.
Second, use reliable interaction checkers. Websites like Drugs.com or apps such as Medisafe let you enter multiple medications and flag potential problems. Remember, these tools are a guide, not a substitute for professional advice.
Third, talk to a pharmacist whenever you start a new drug or supplement. Pharmacists have access to up‑to‑date interaction databases and can suggest timing tweaks or safer alternatives. If your doctor prescribes a new medication, ask them to review your current list; a quick review can prevent a nasty surprise.
Lastly, monitor how you feel. If you notice new symptoms—headaches, rash, stomach upset, or unusual fatigue—note the timing and report it immediately. Early detection means you can adjust the regimen before the issue escalates.
Drug interactions are a real risk, but they’re manageable with a bit of organization and the right questions. Keep your list, use a checker, and keep the conversation open with your healthcare team. By staying proactive, you’ll get the full benefit of each medication without unwanted side effects.

Seizure Medications and Pregnancy: Birth Defect Risks and Drug Interactions You Need to Know
Feb, 1 2026
Omeprazole and Clopidogrel: How CYP2C19 Inhibition Affects Heart Drug Effectiveness
Nov, 2 2025
How to Read the Safety and Warnings Sections of Prescription Drug Labels
Oct, 30 2025

Eplerenone and Thyroid Disorders: Essential Patient Guide
Sep, 22 2025
